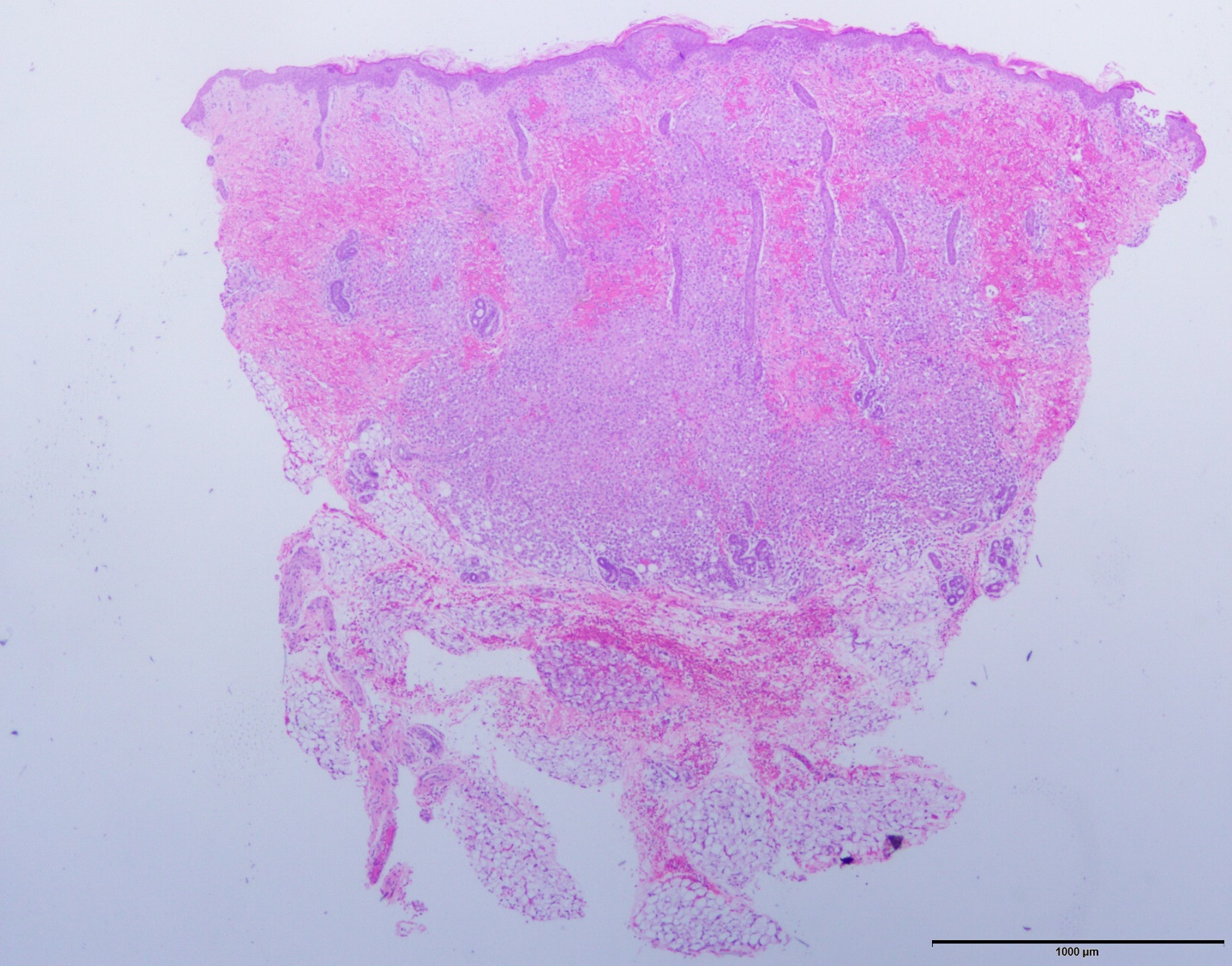
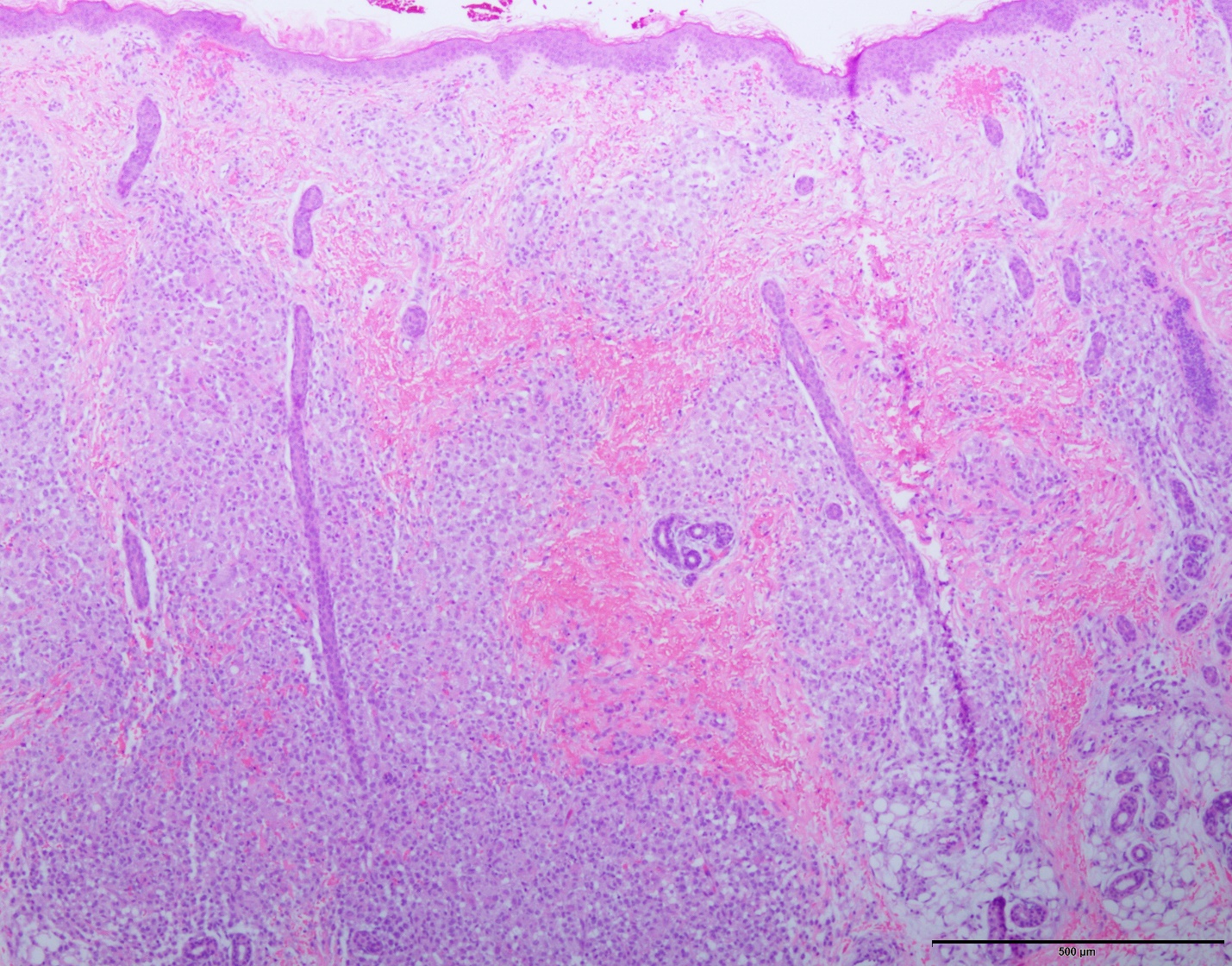
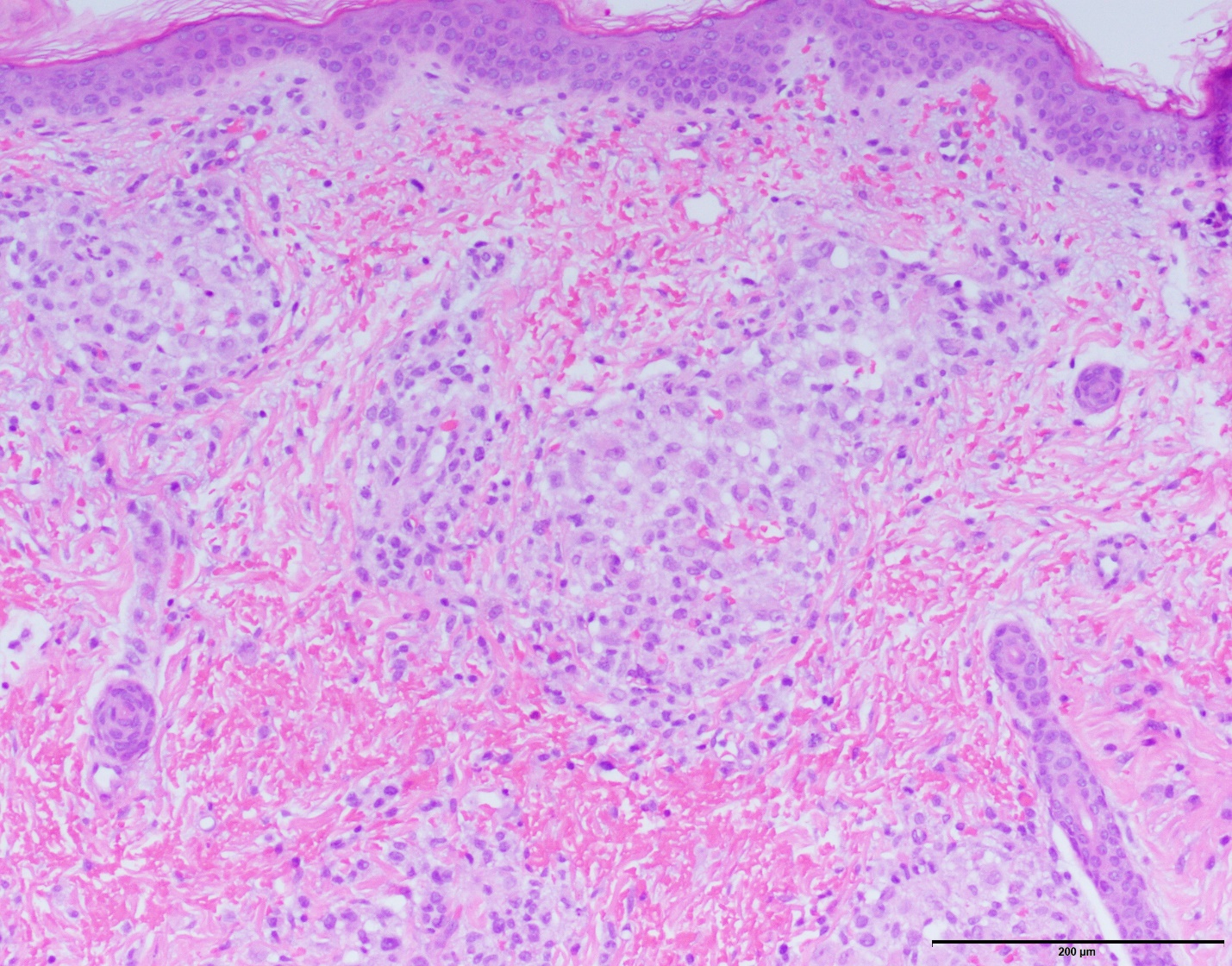
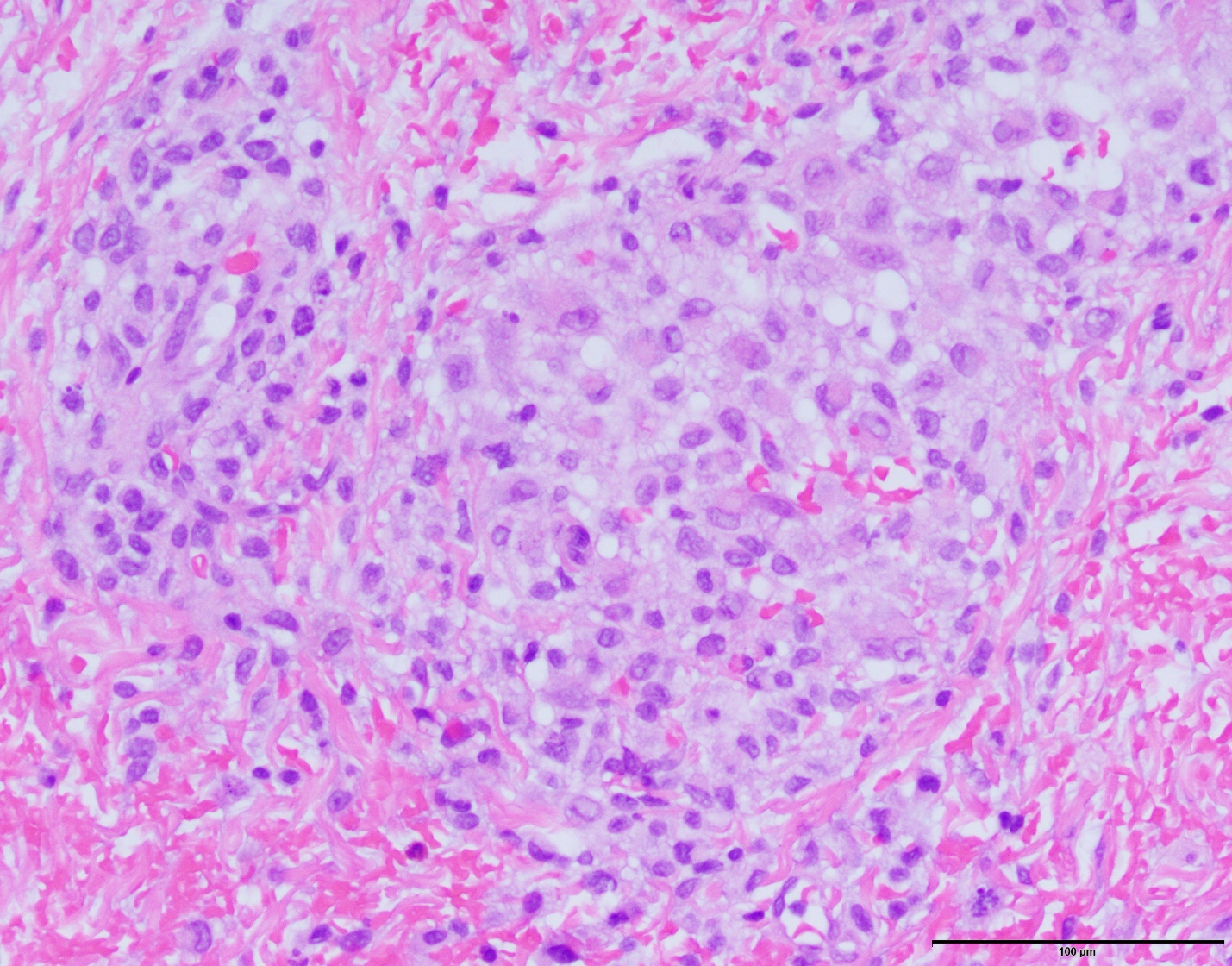
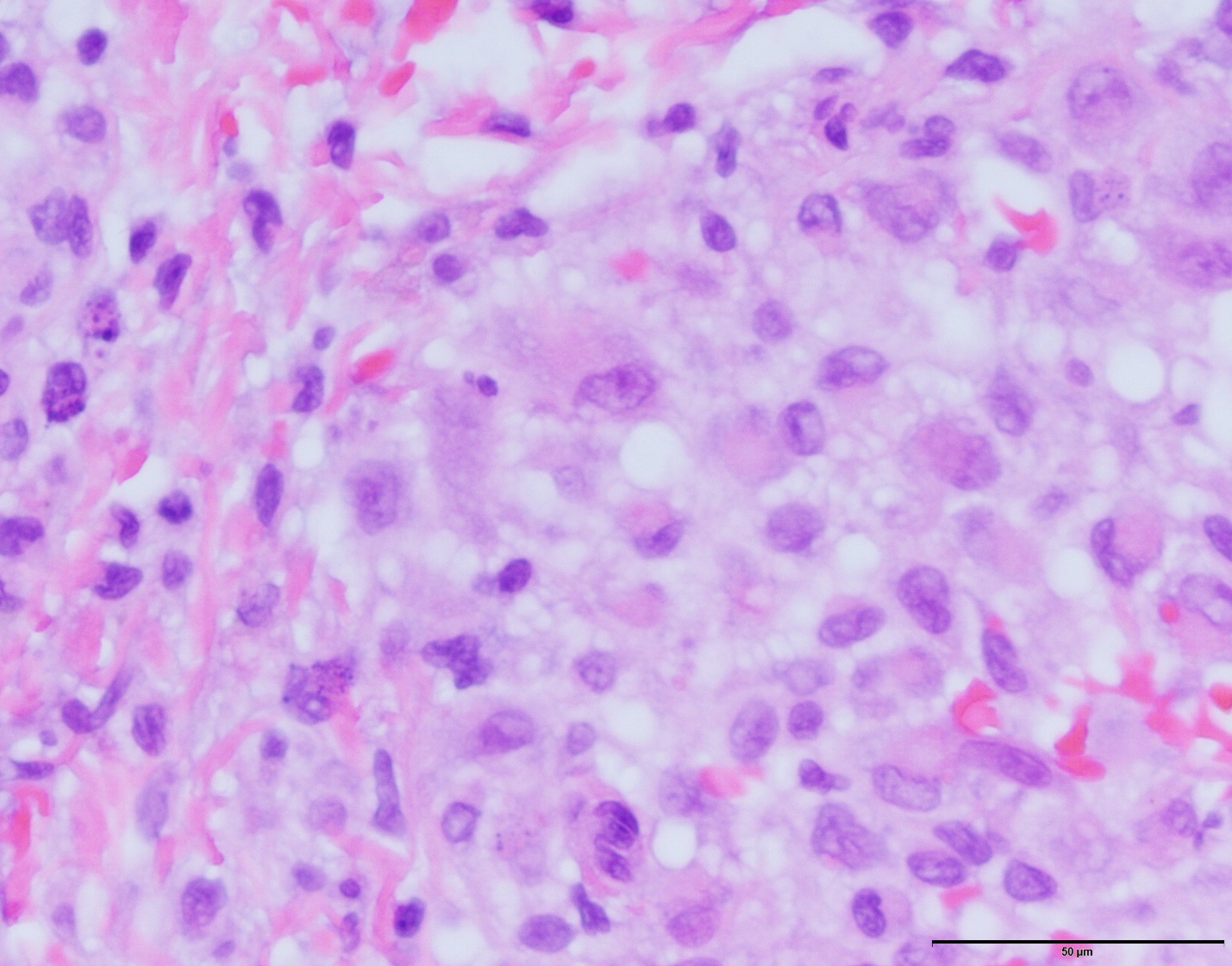
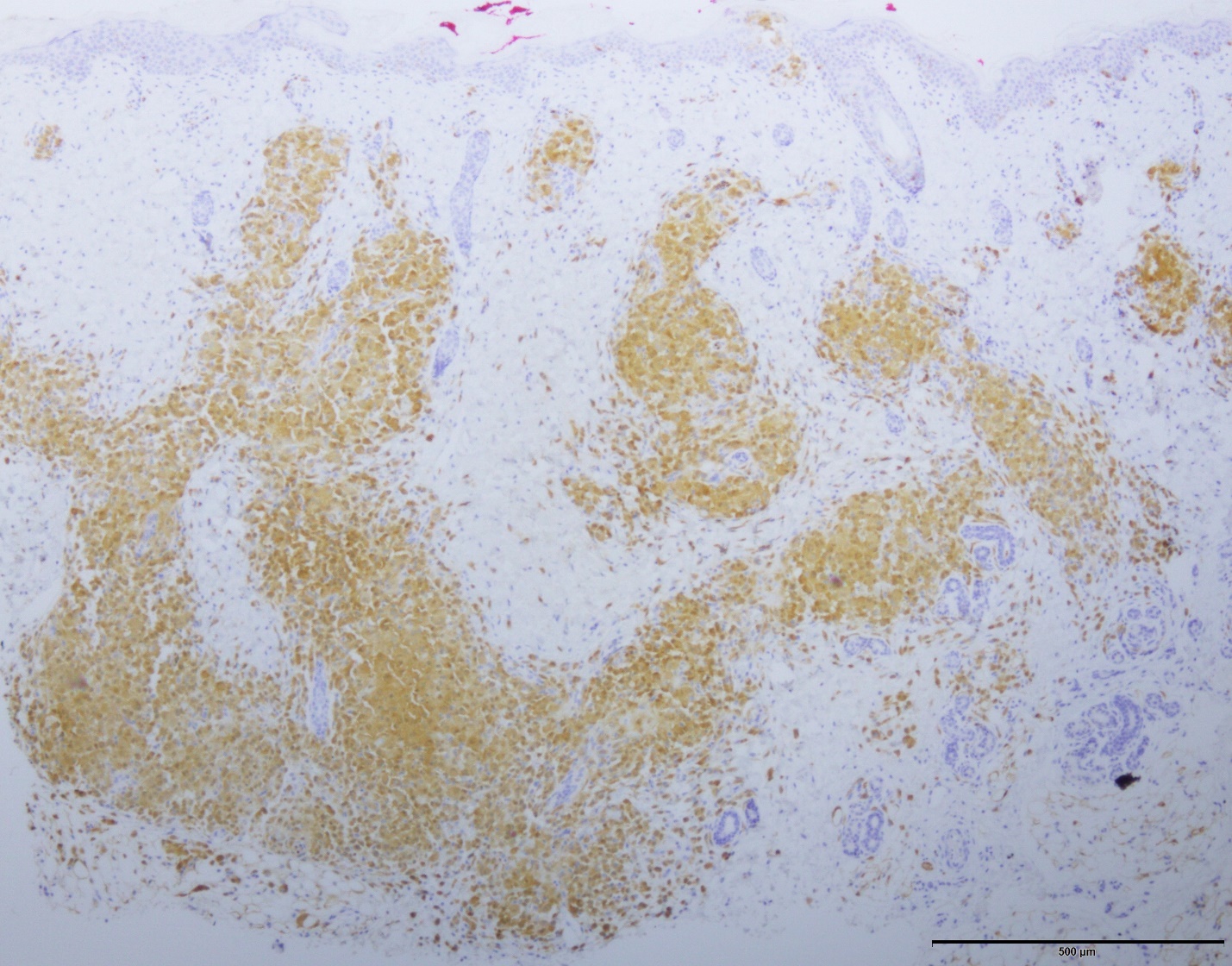
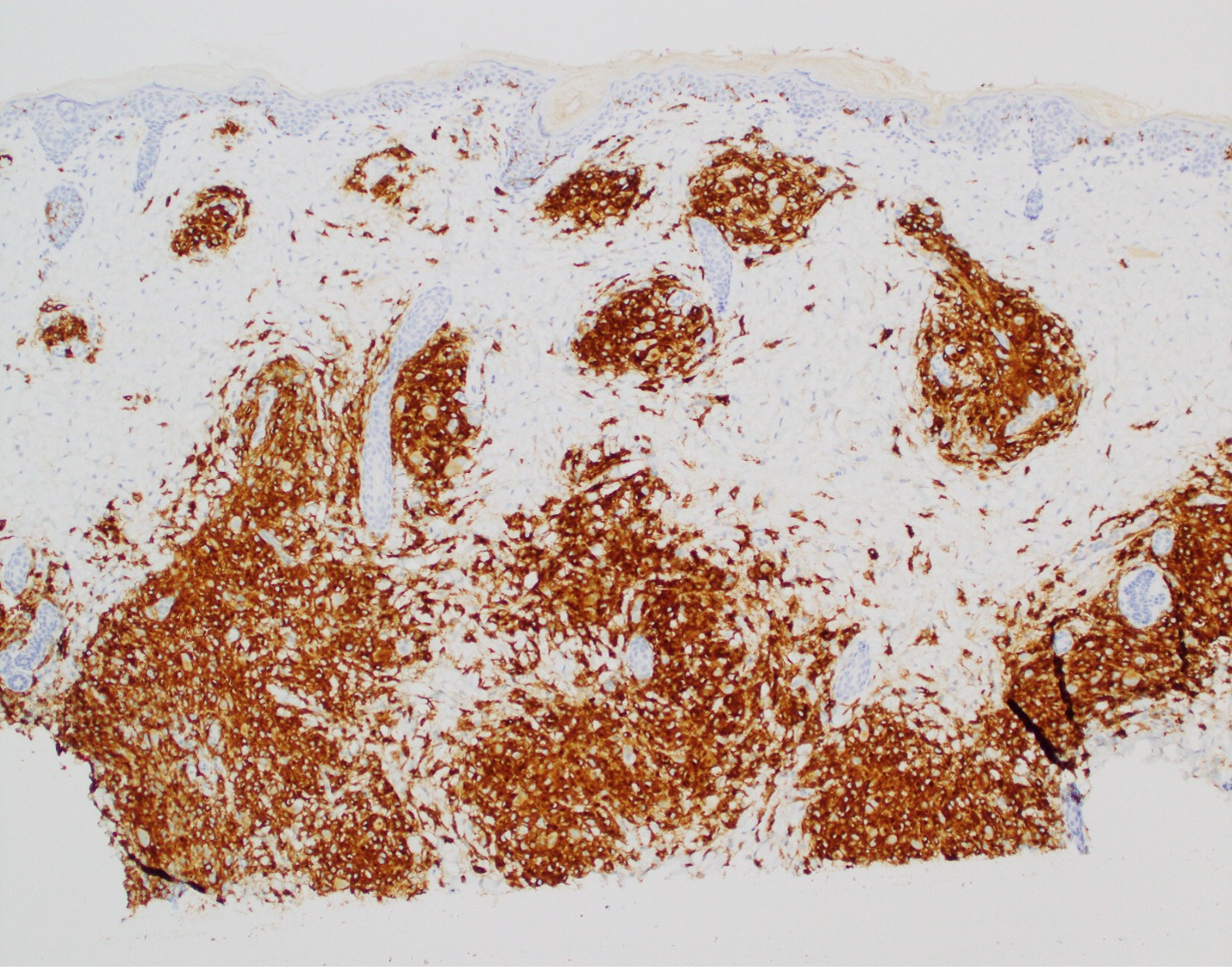
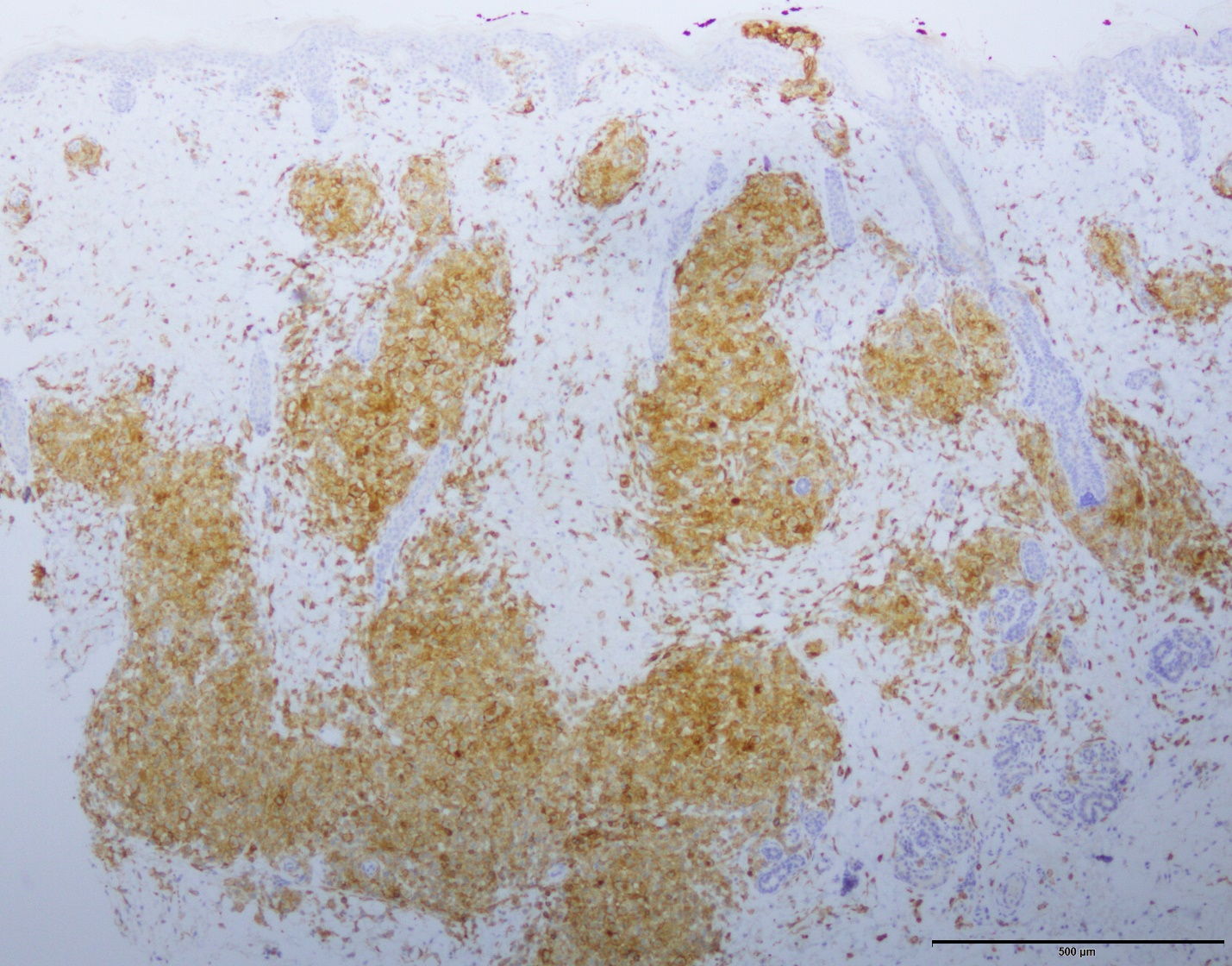
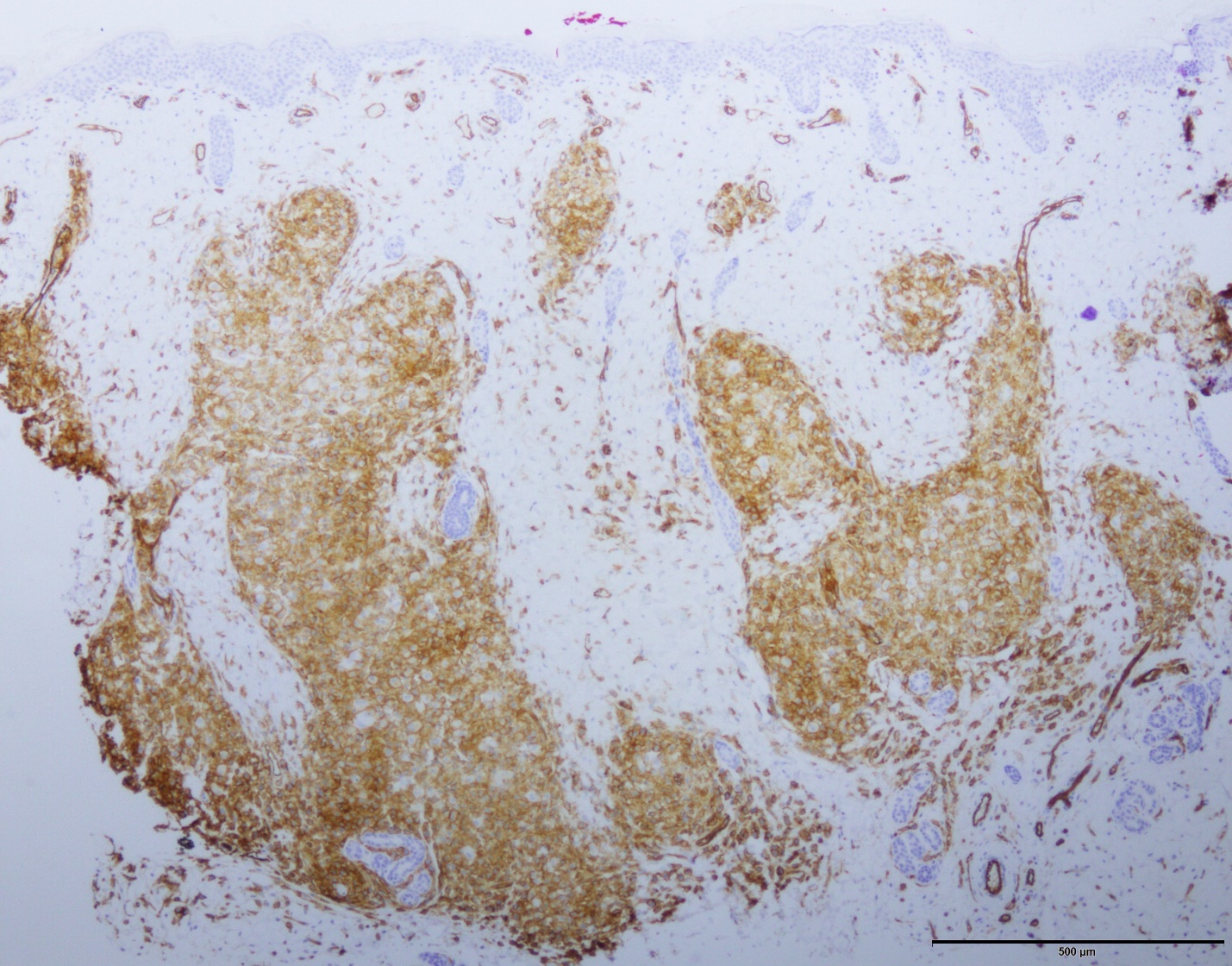
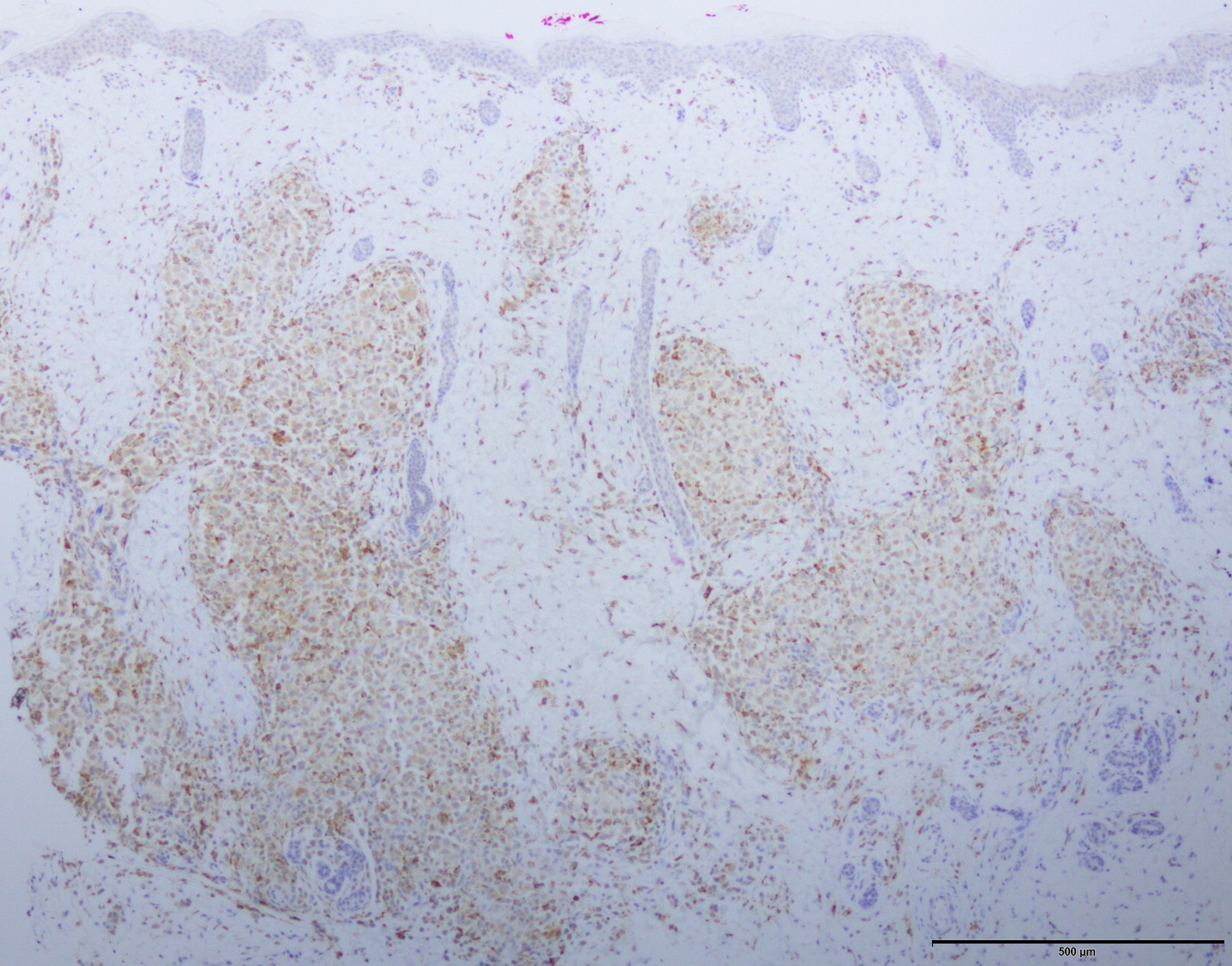
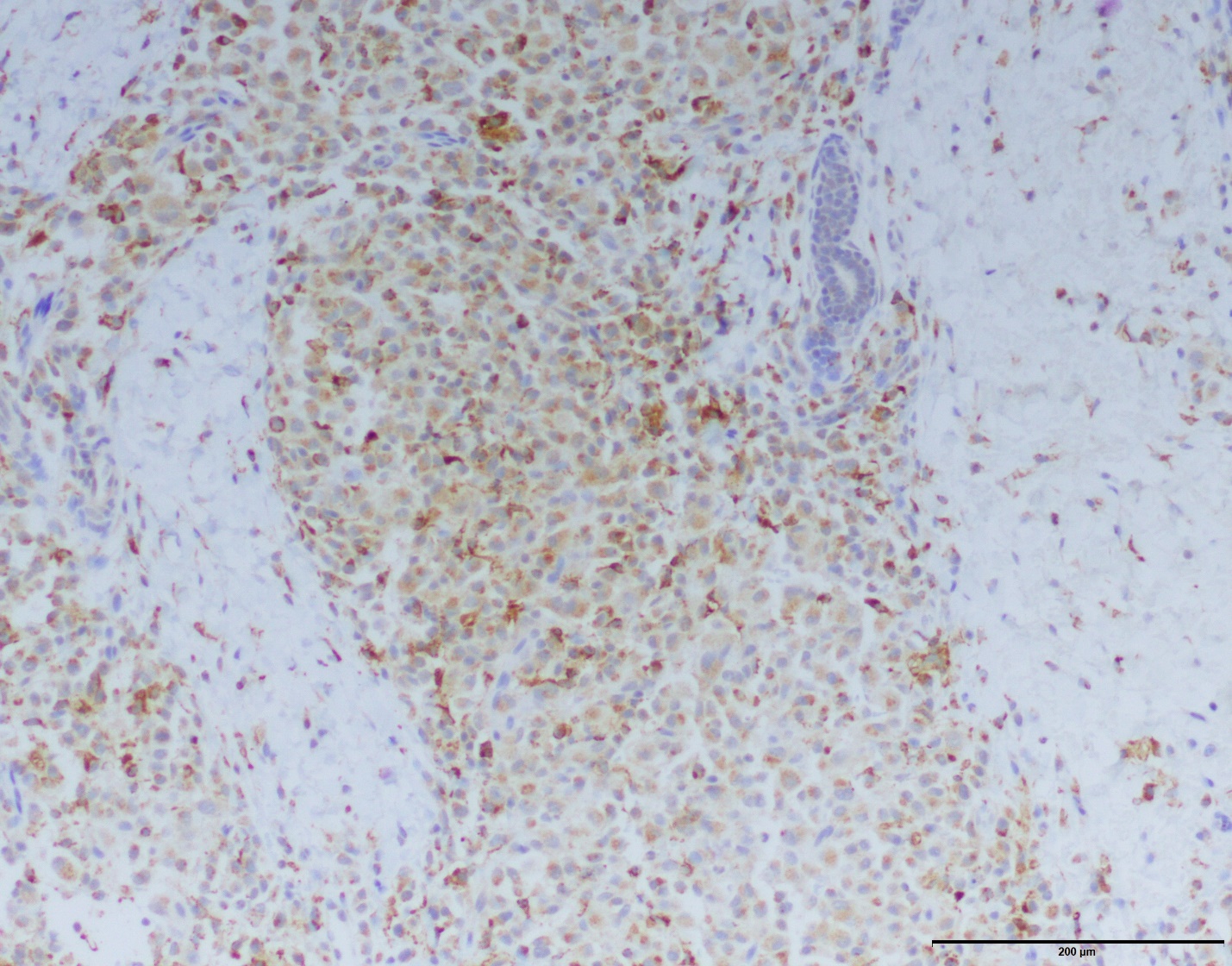
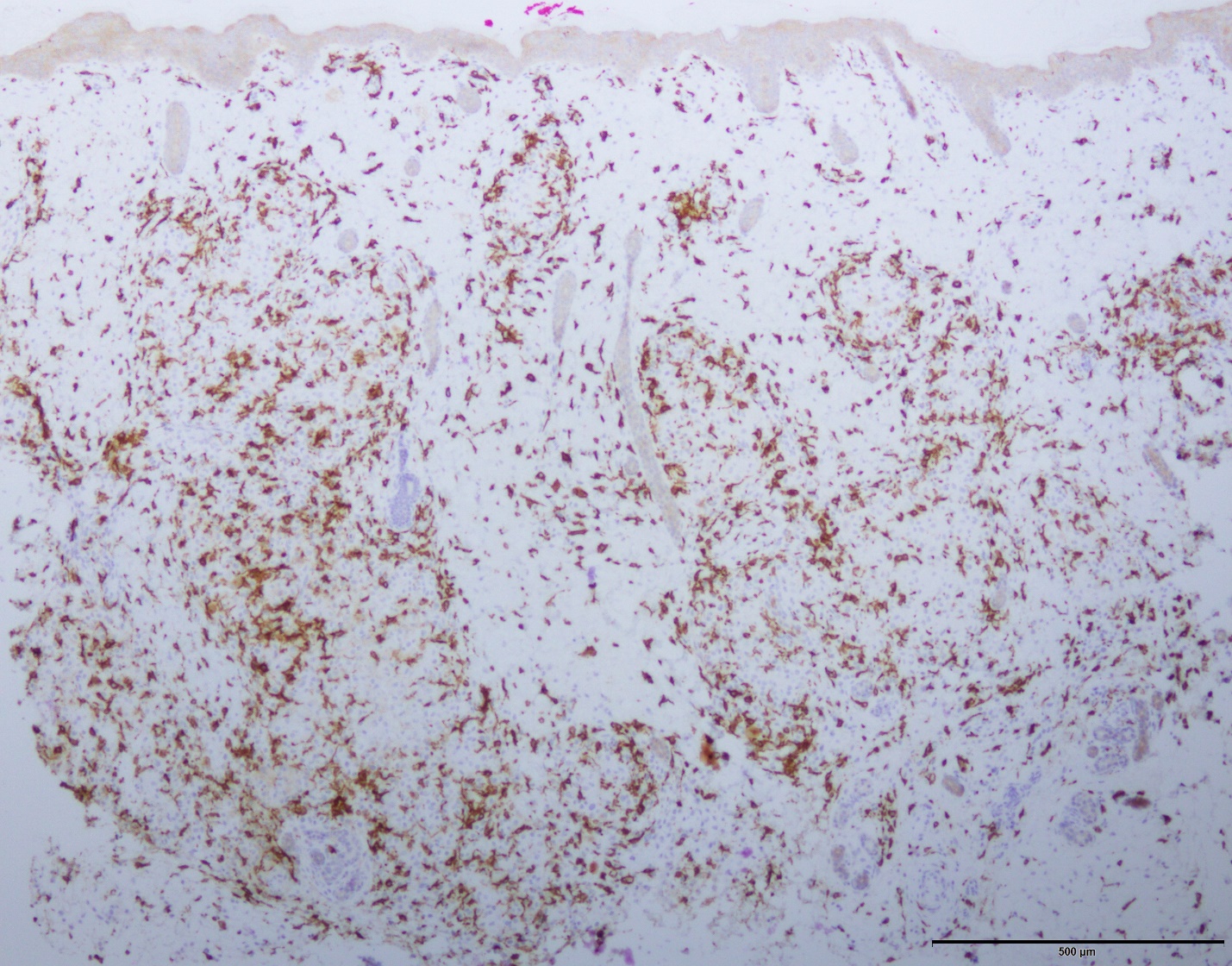
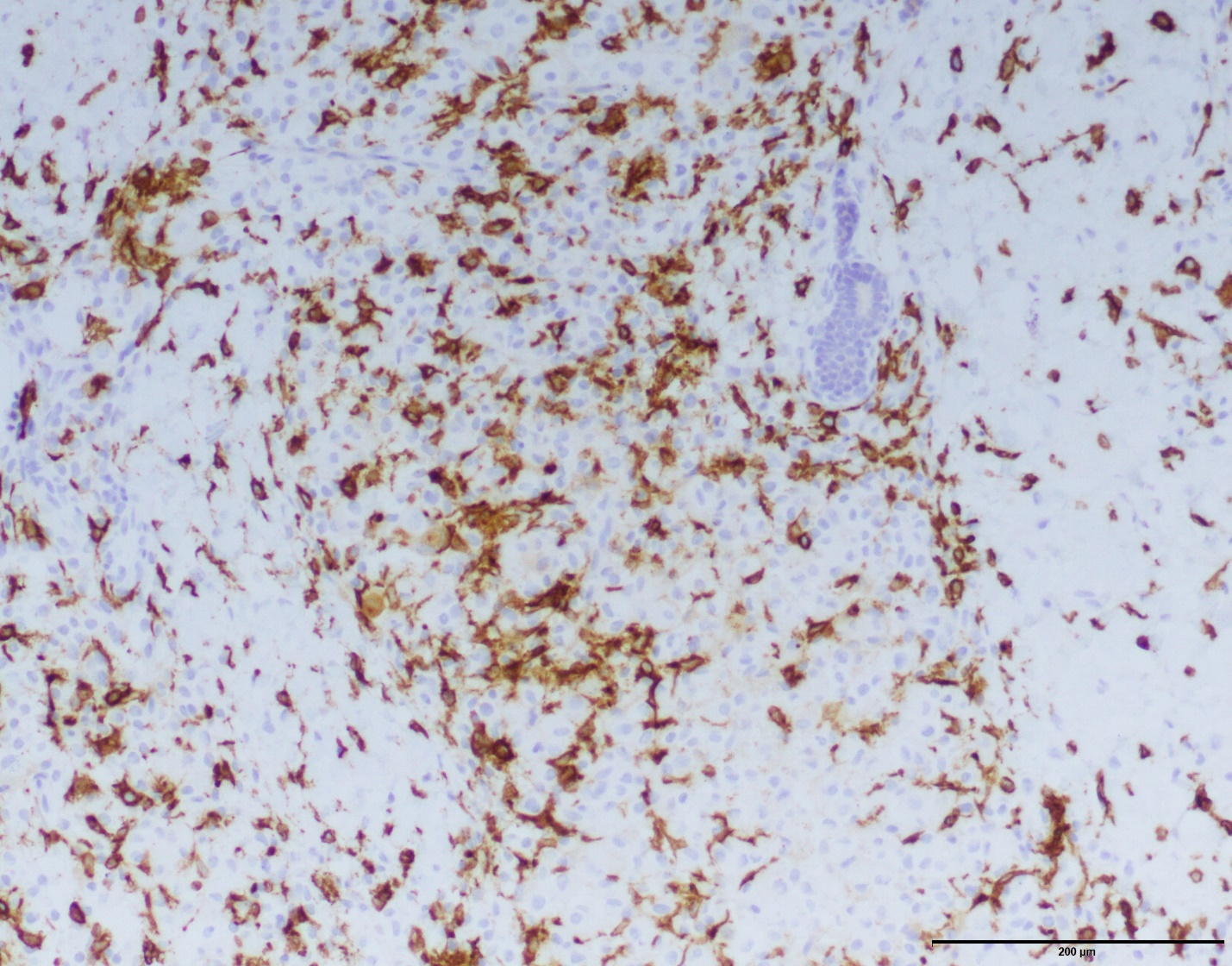
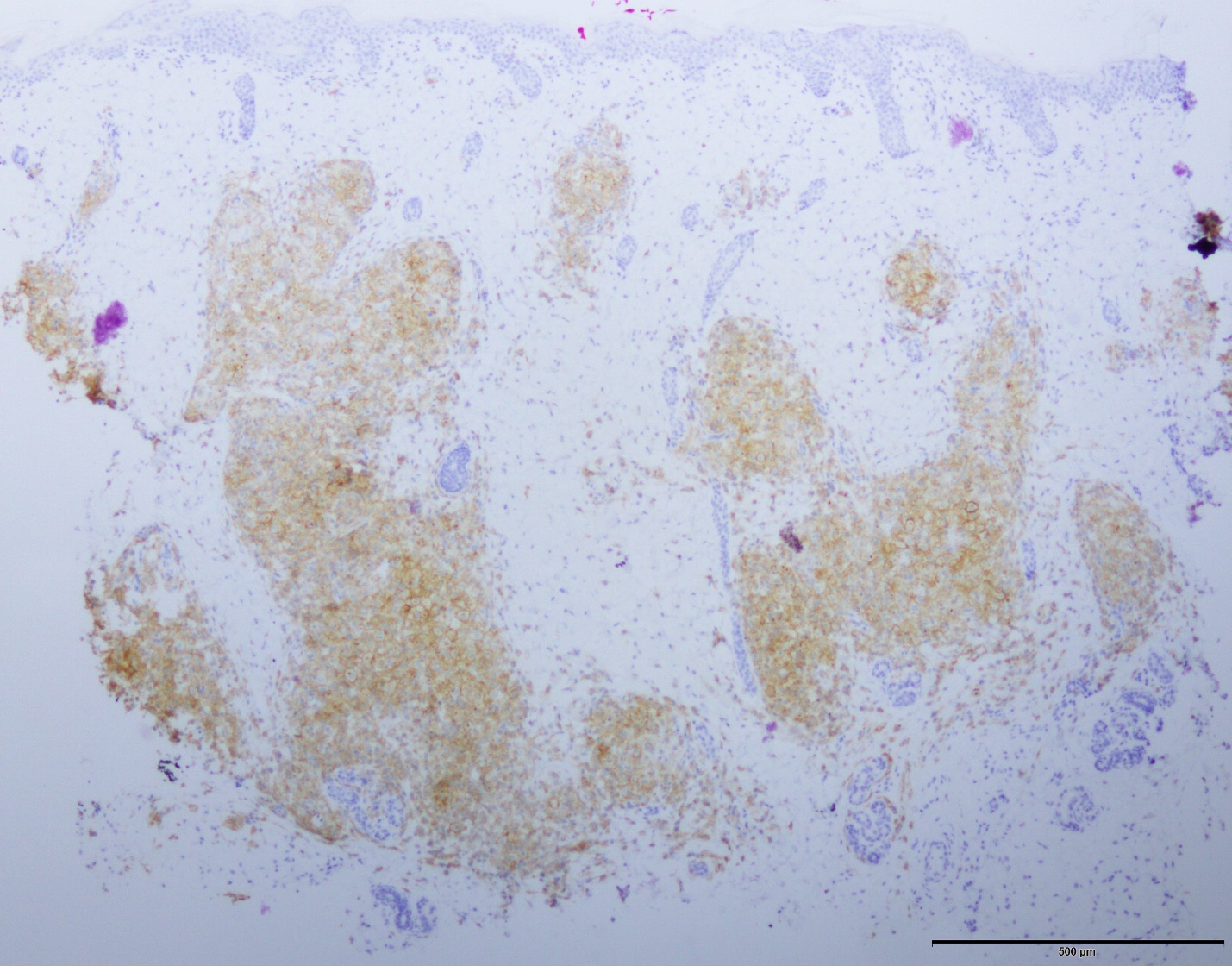
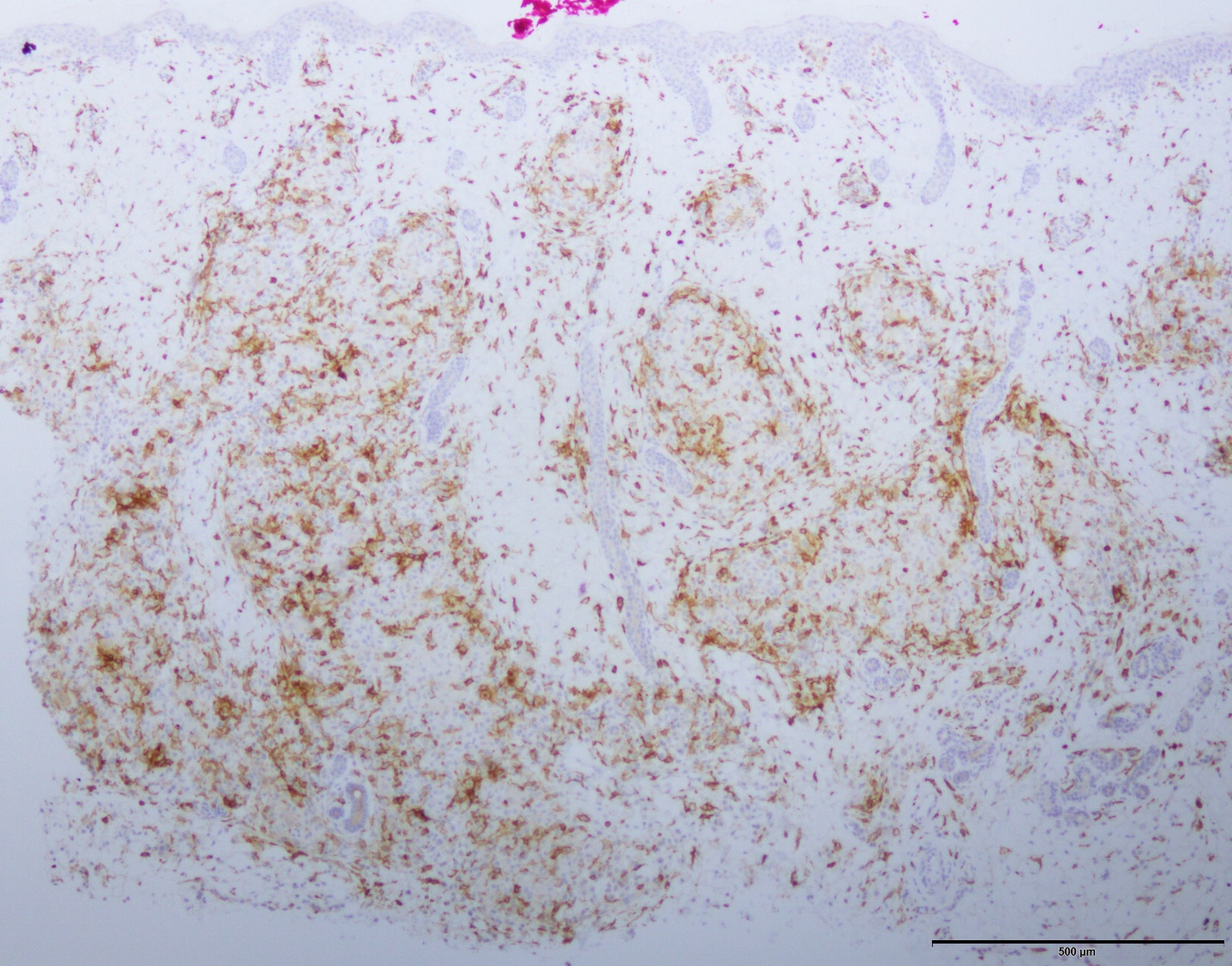
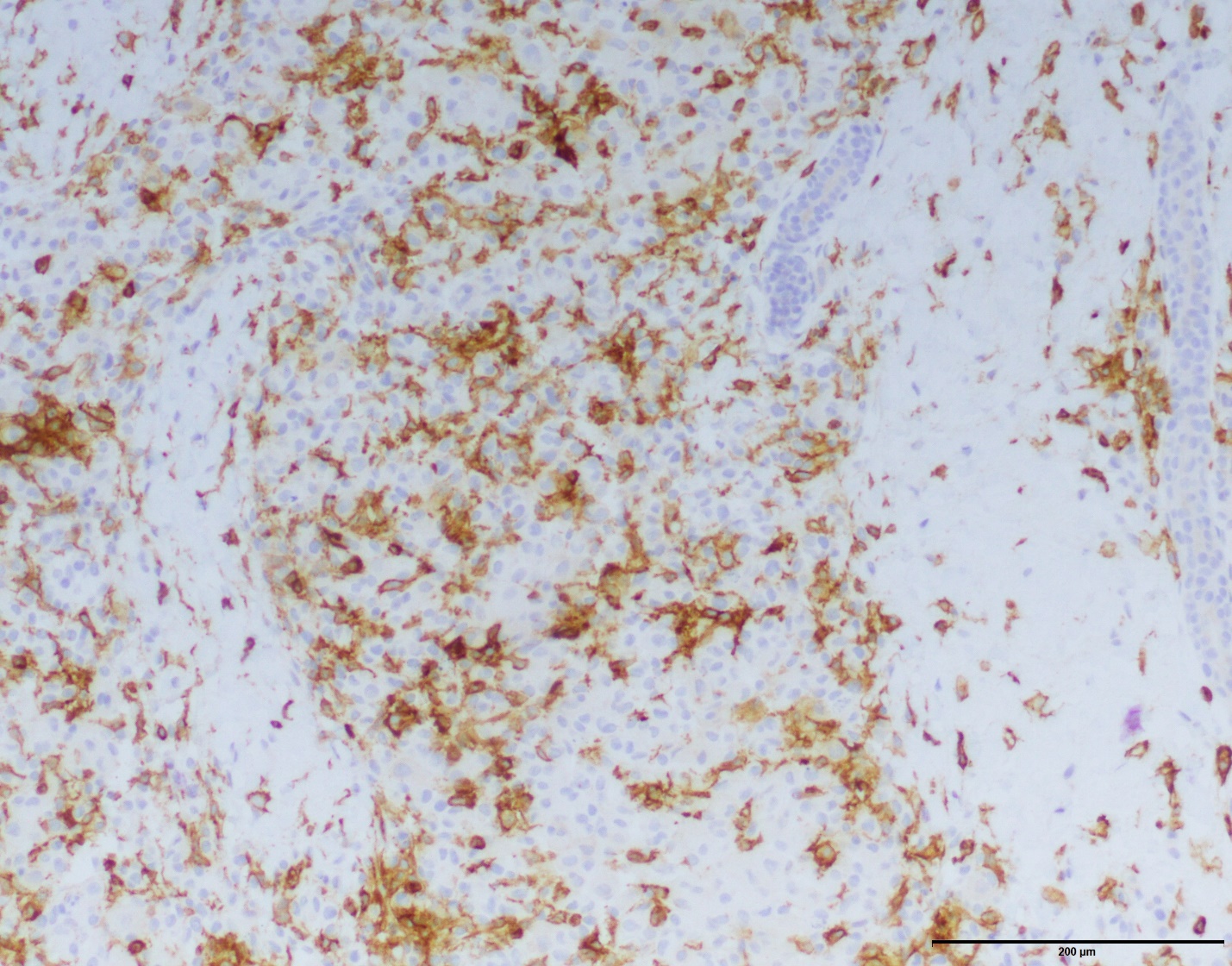
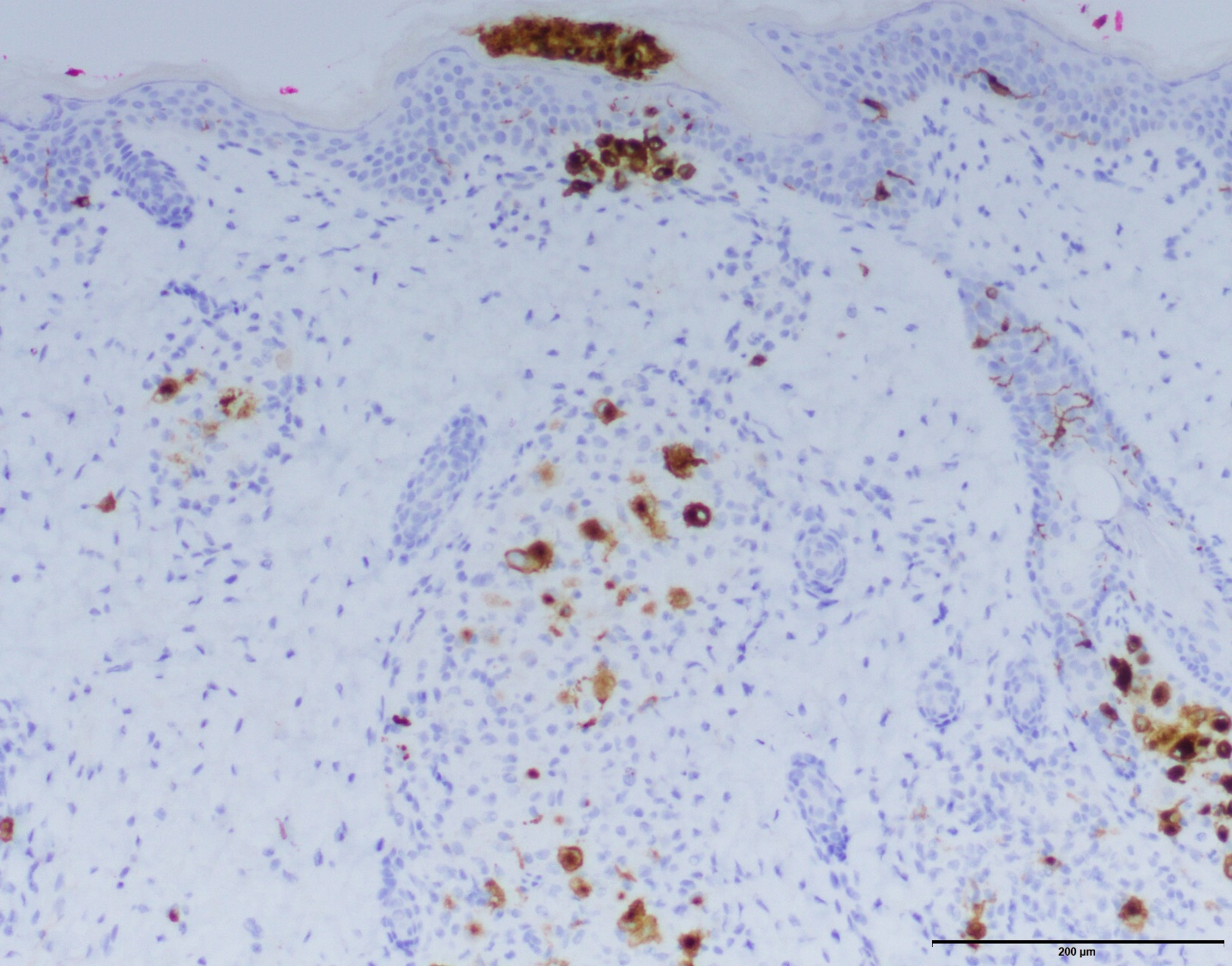
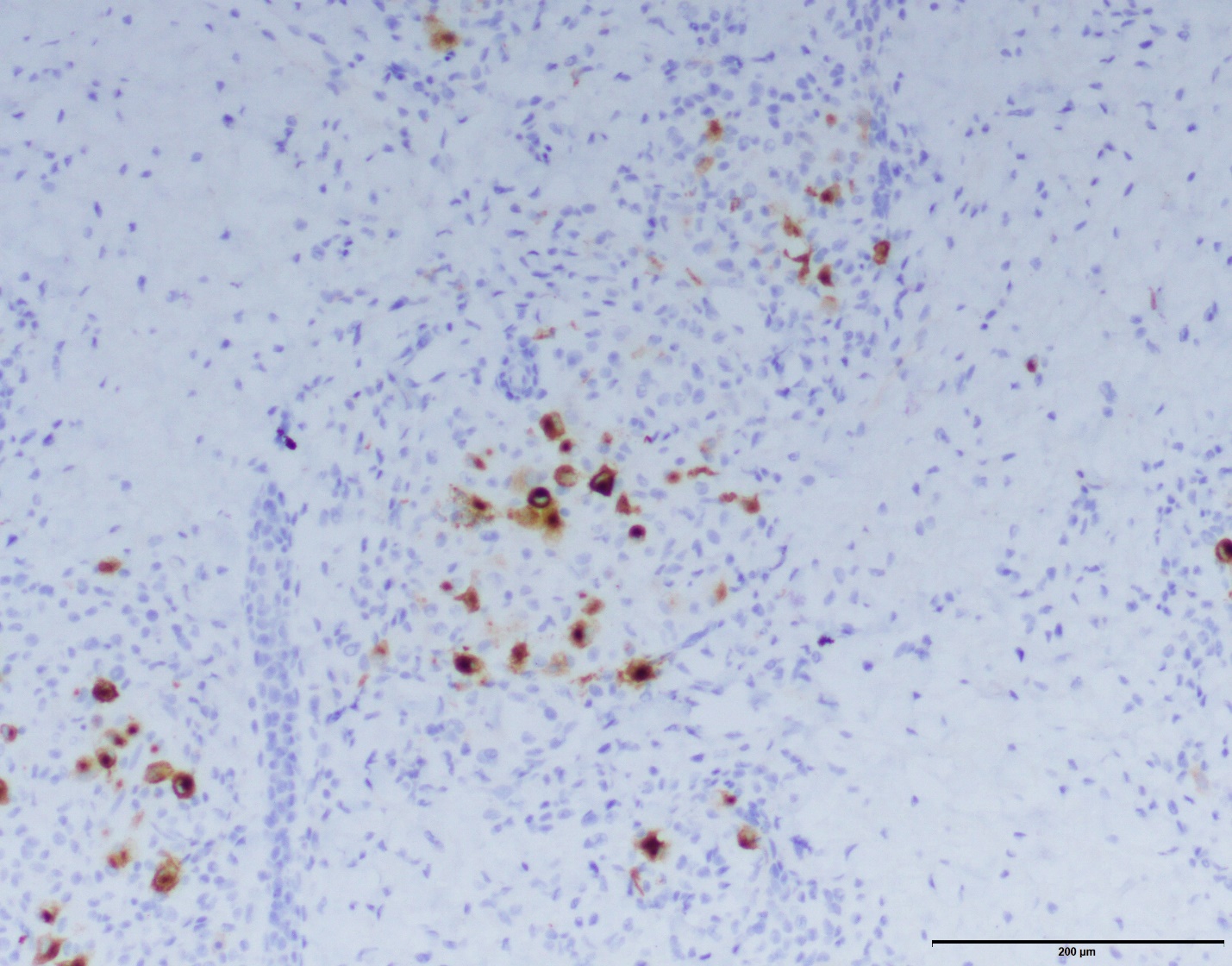
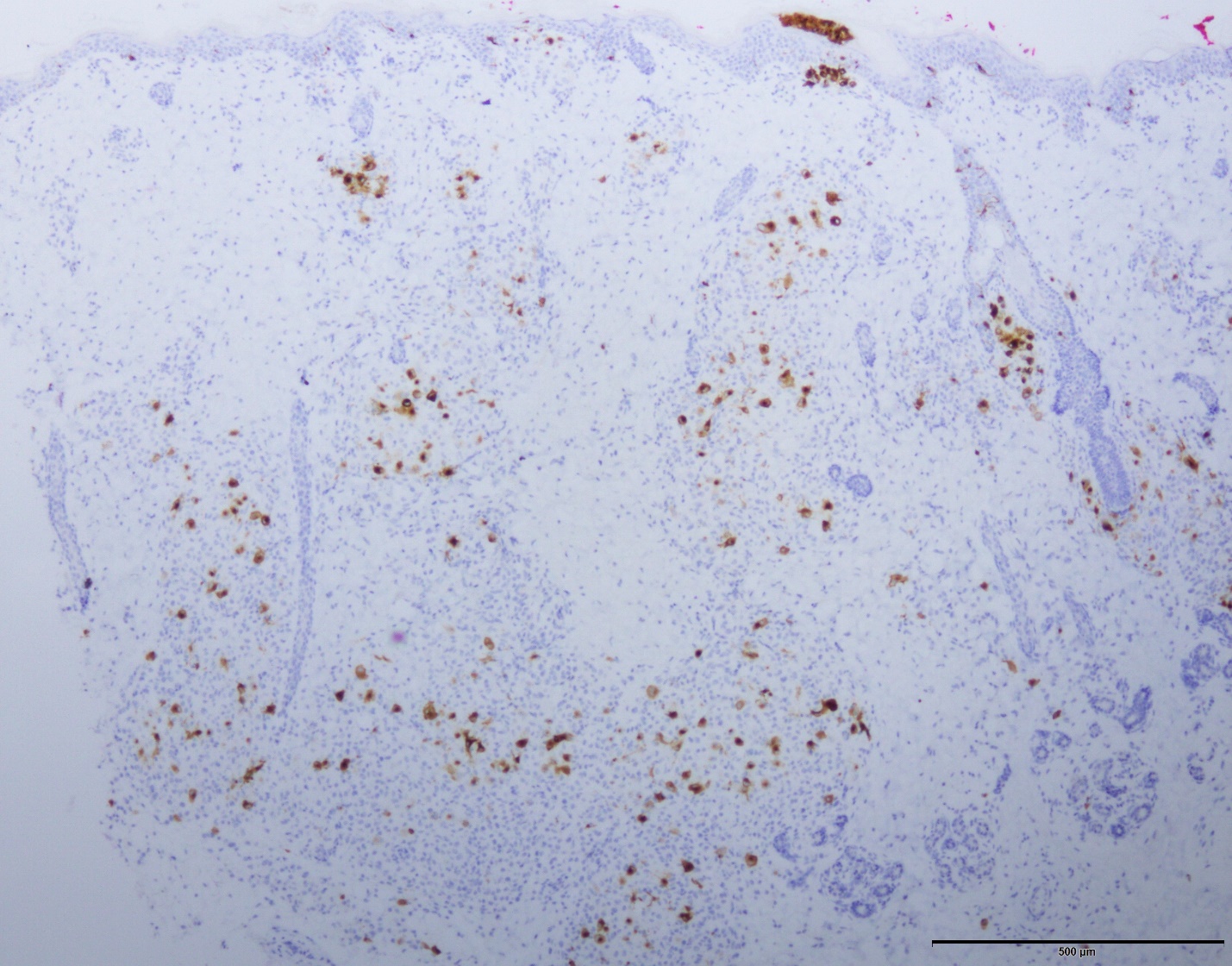
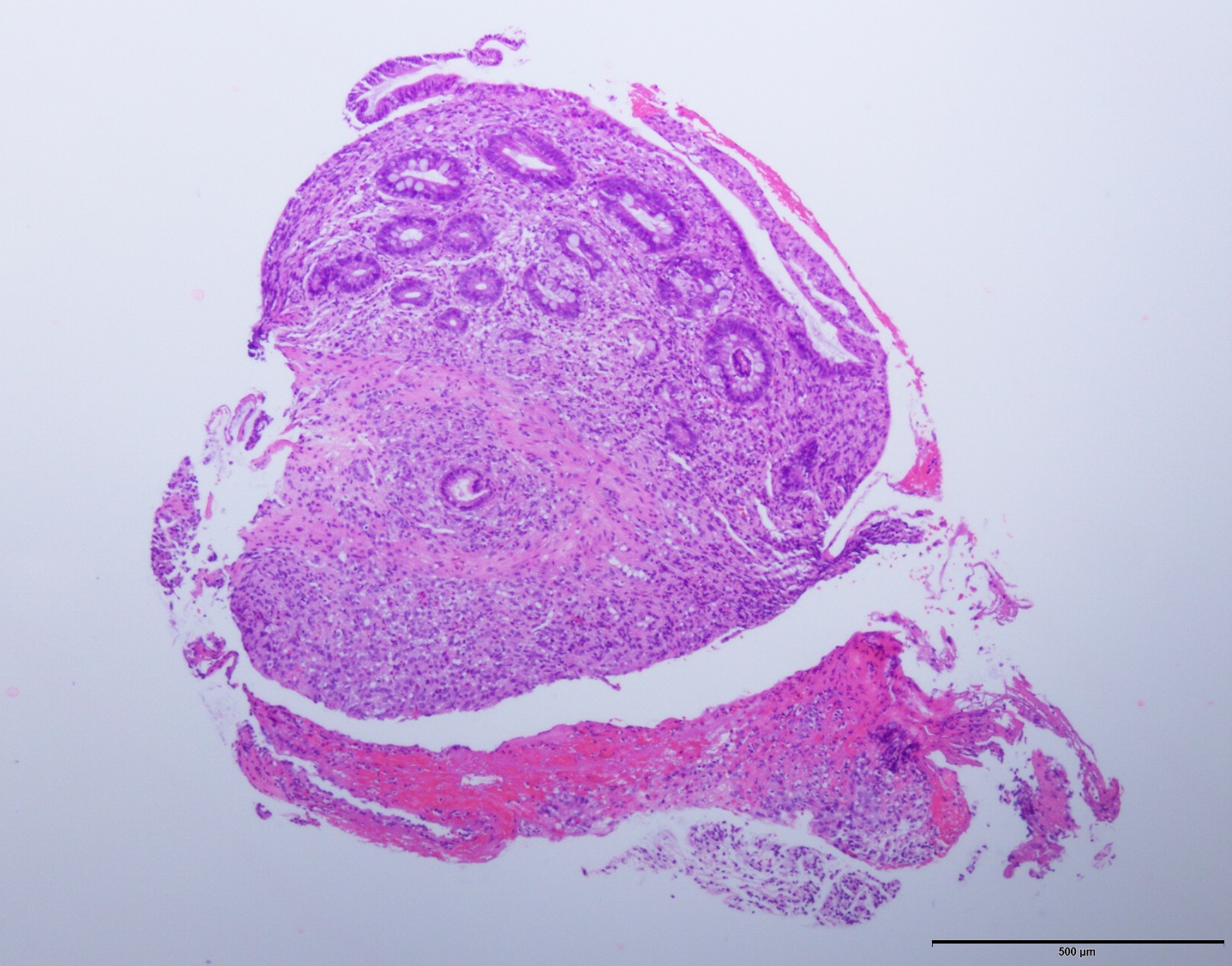
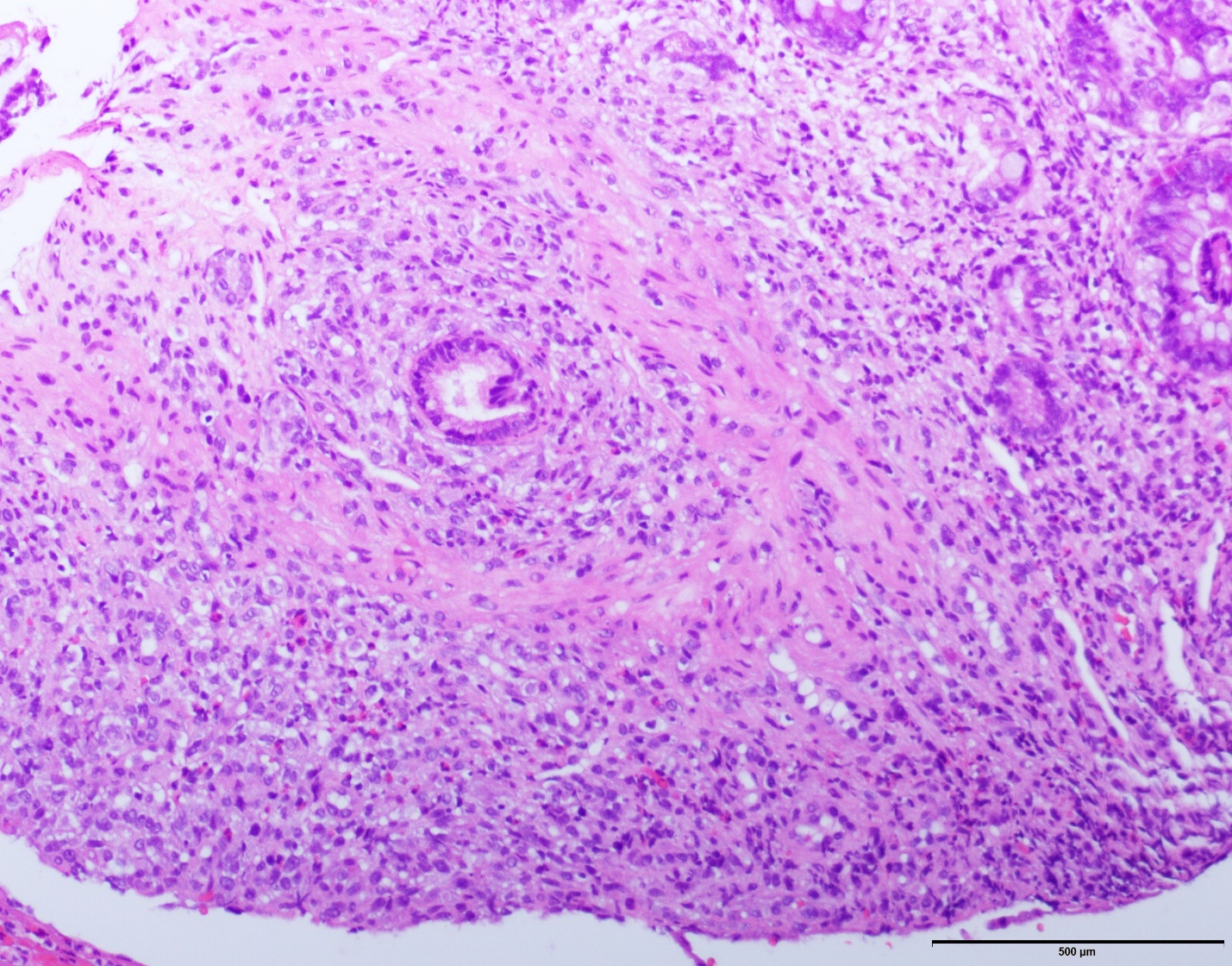
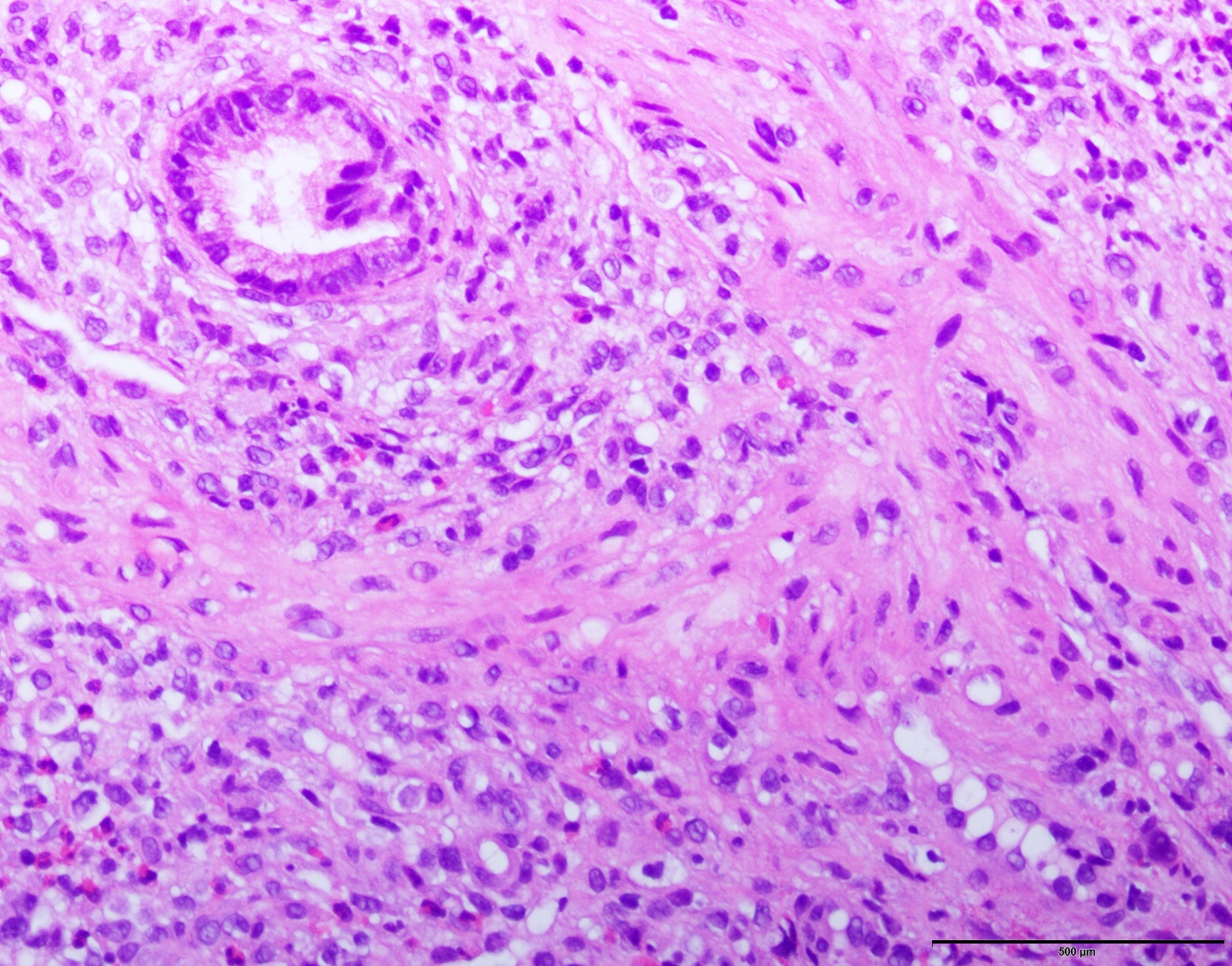
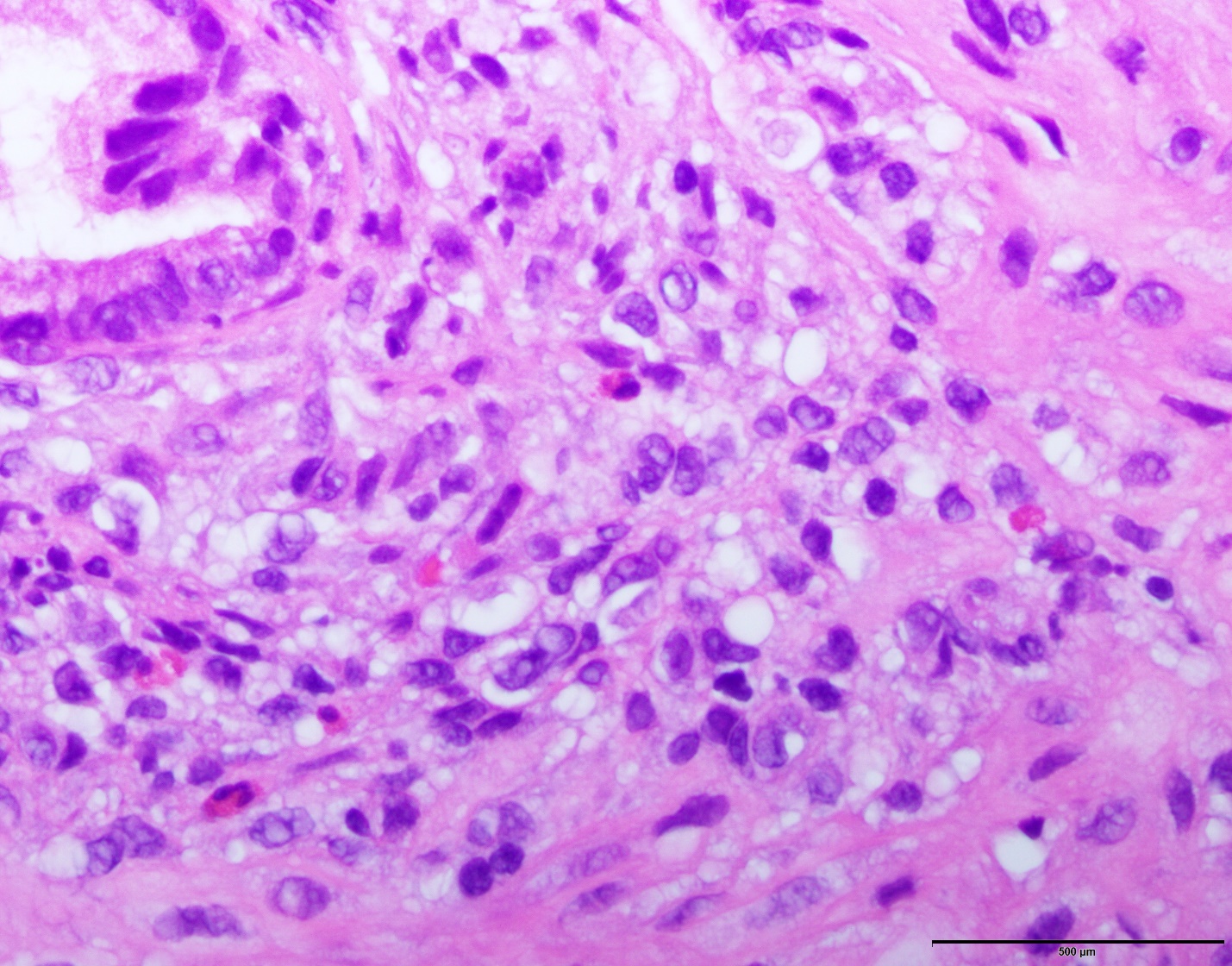
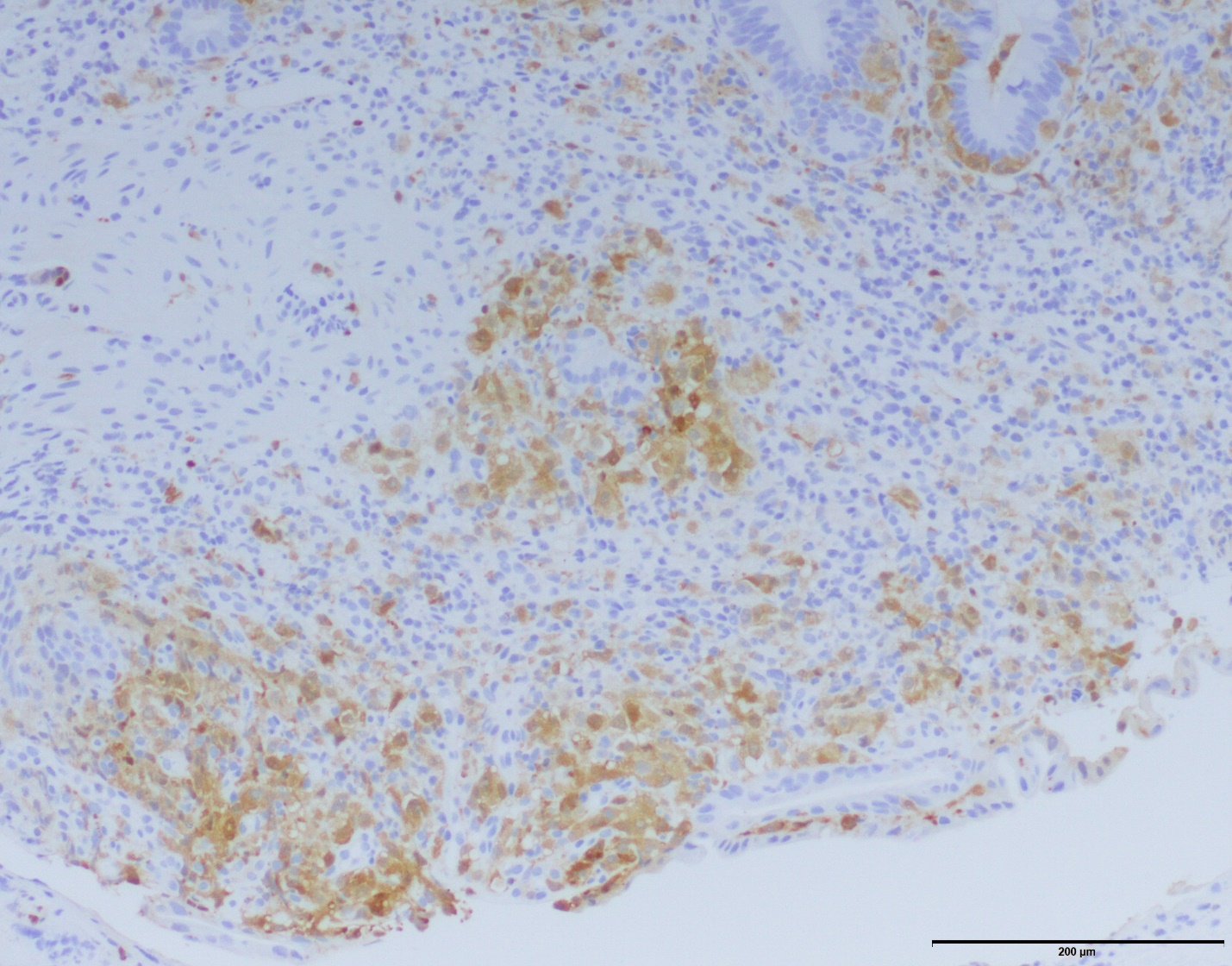
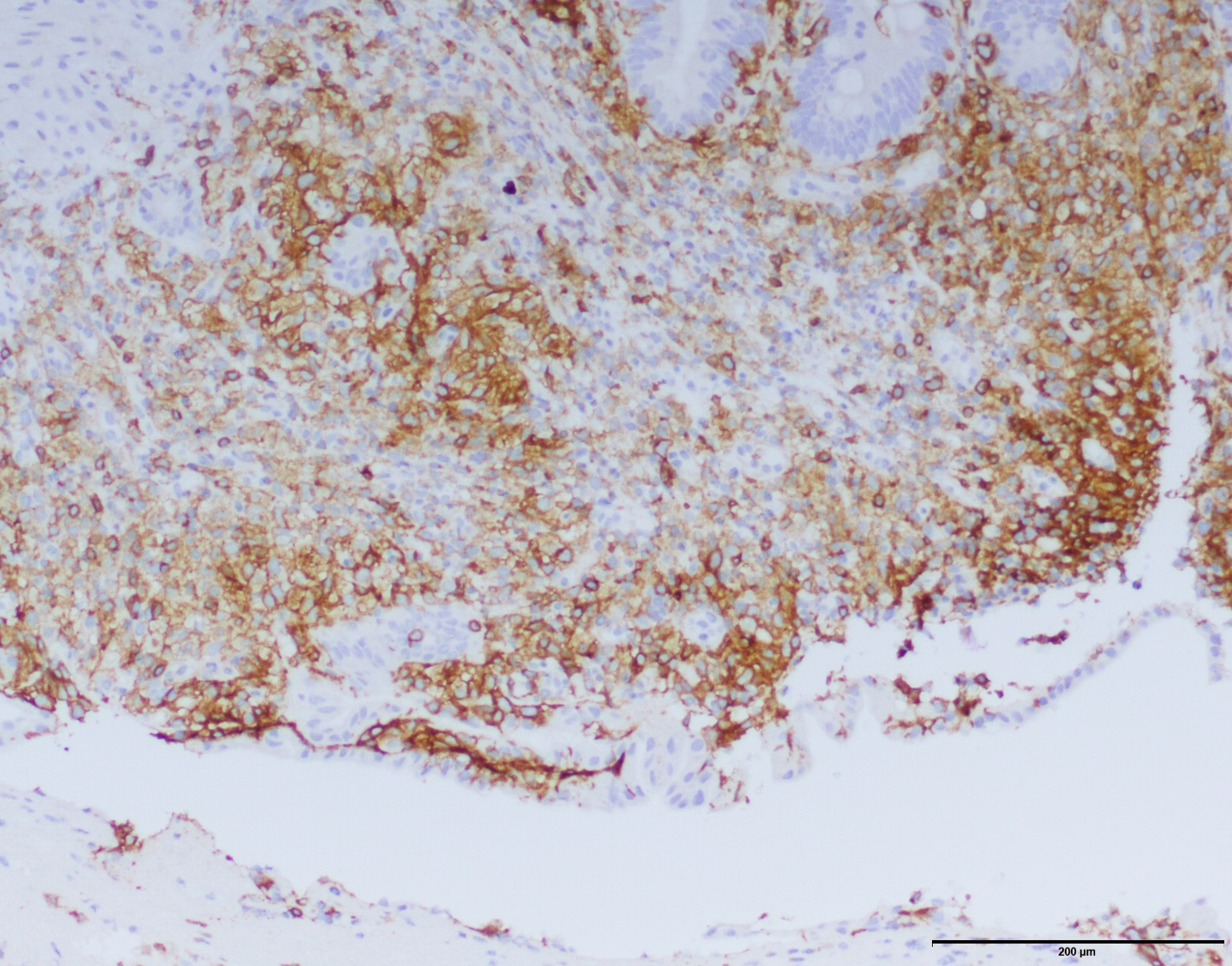
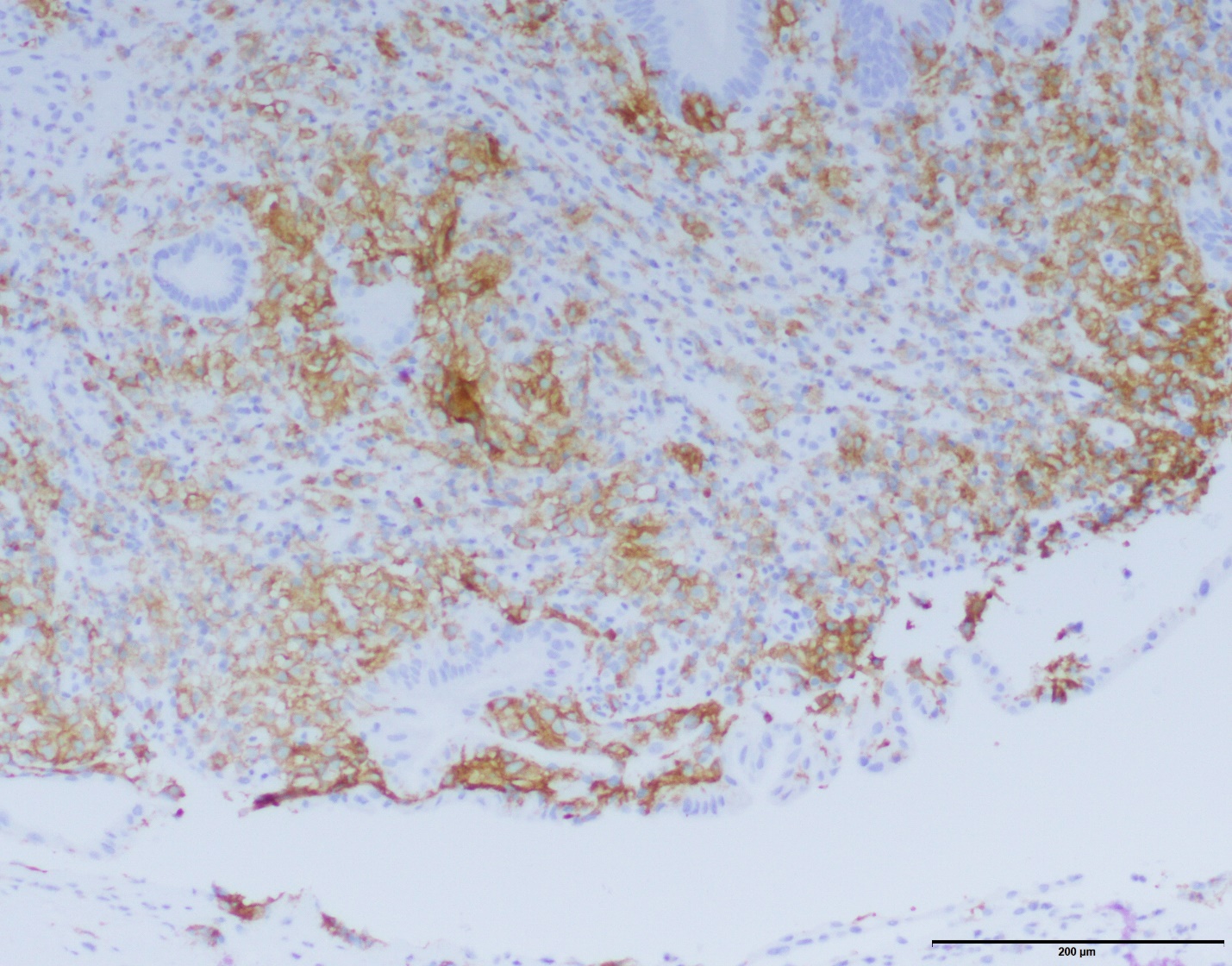
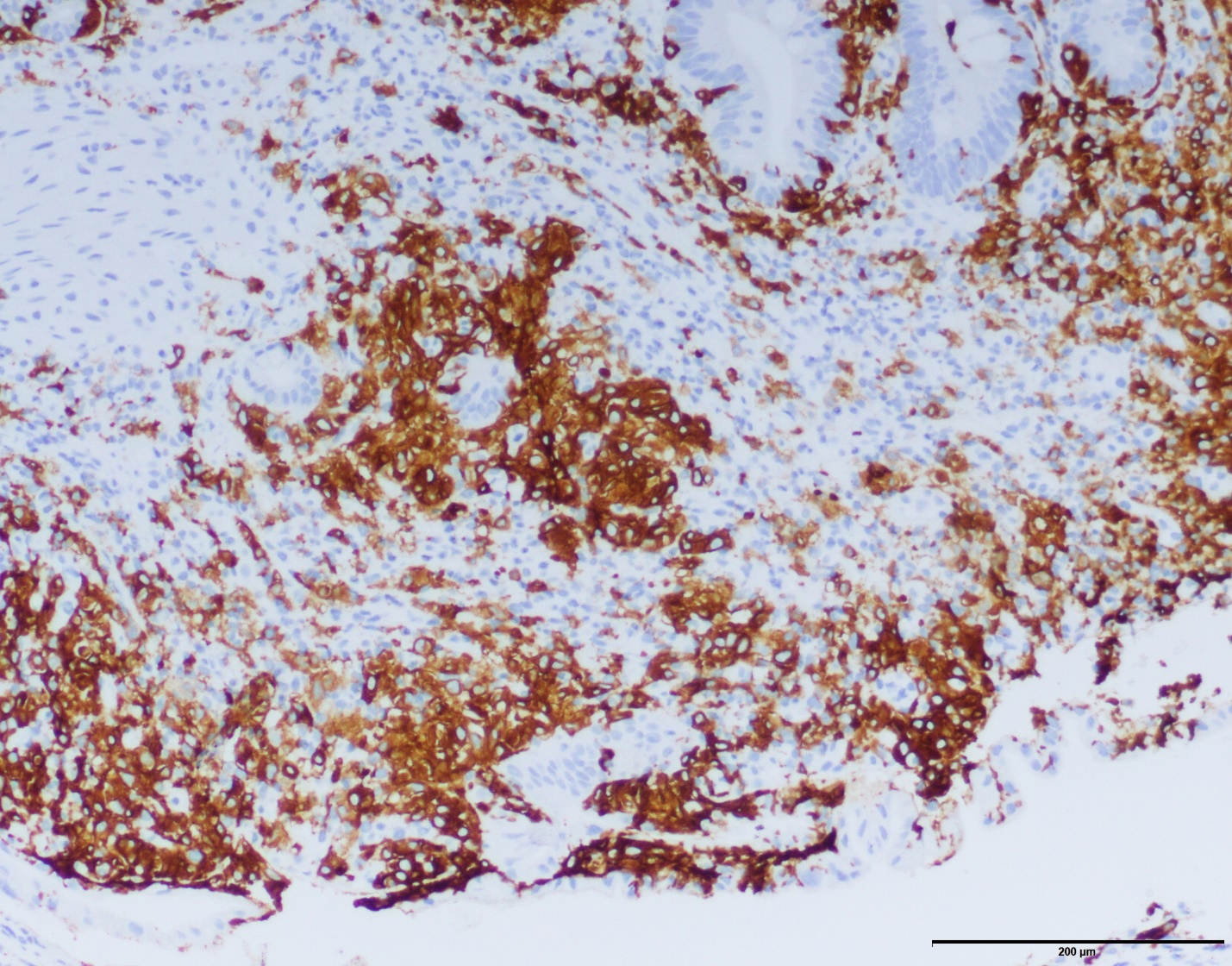
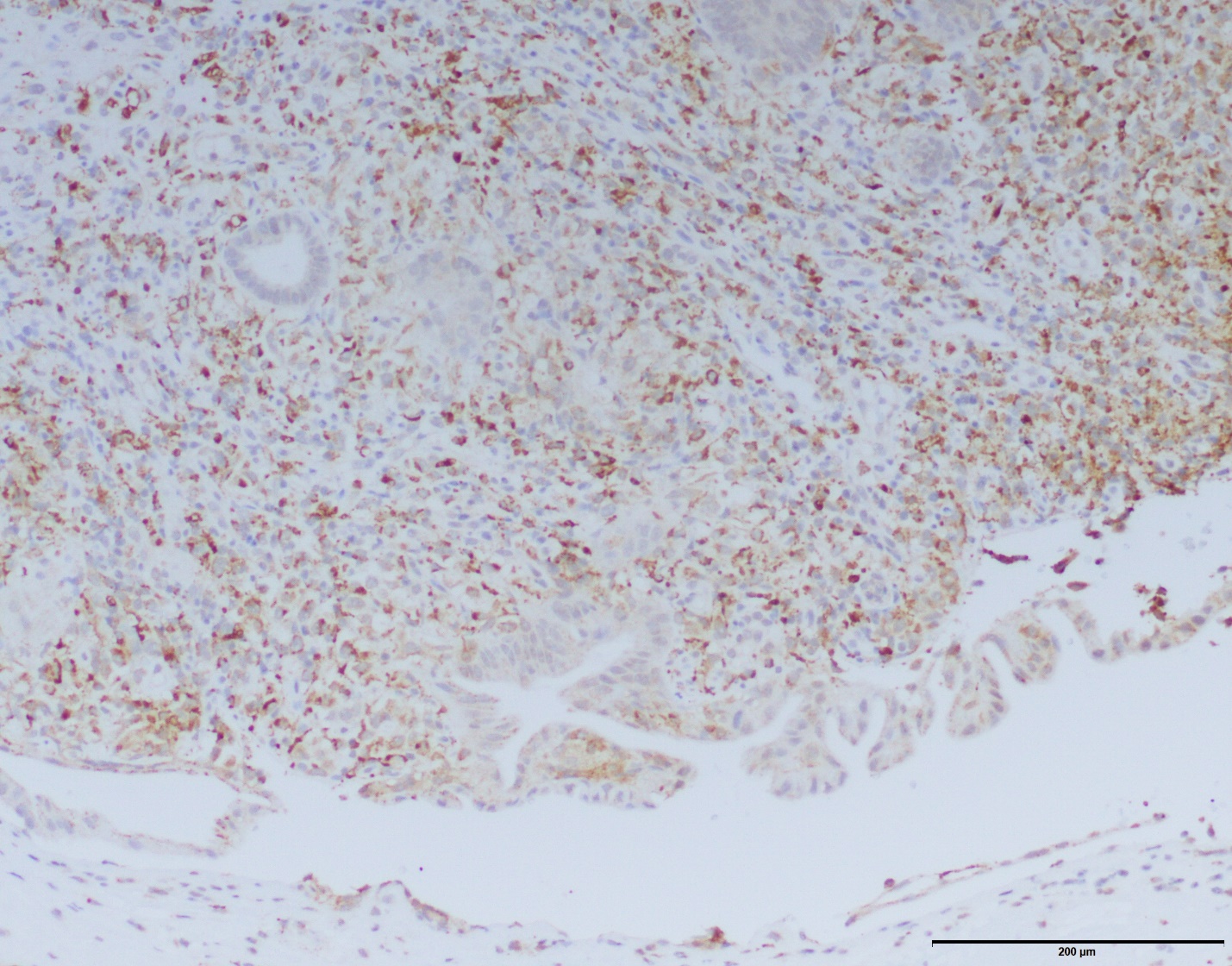
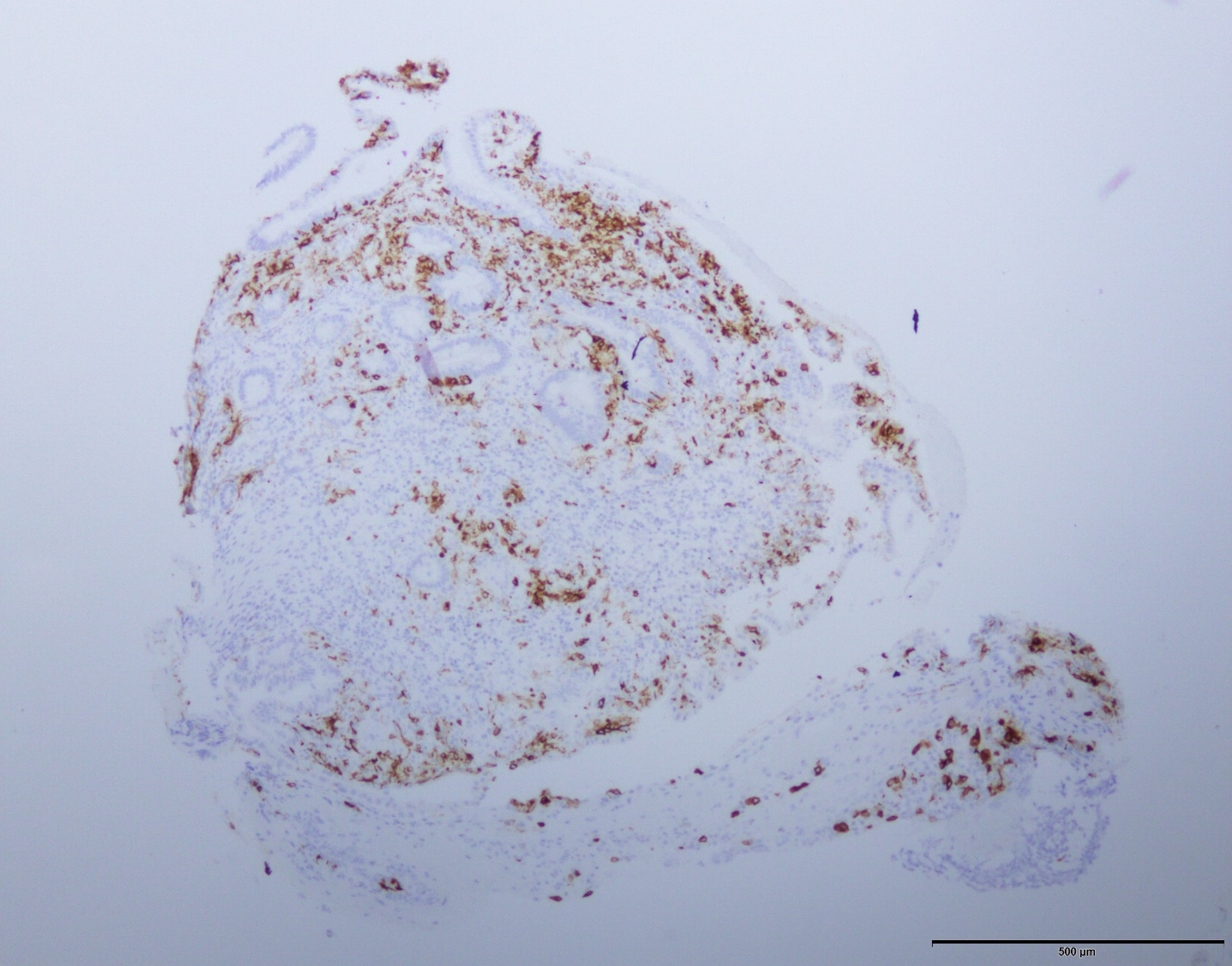
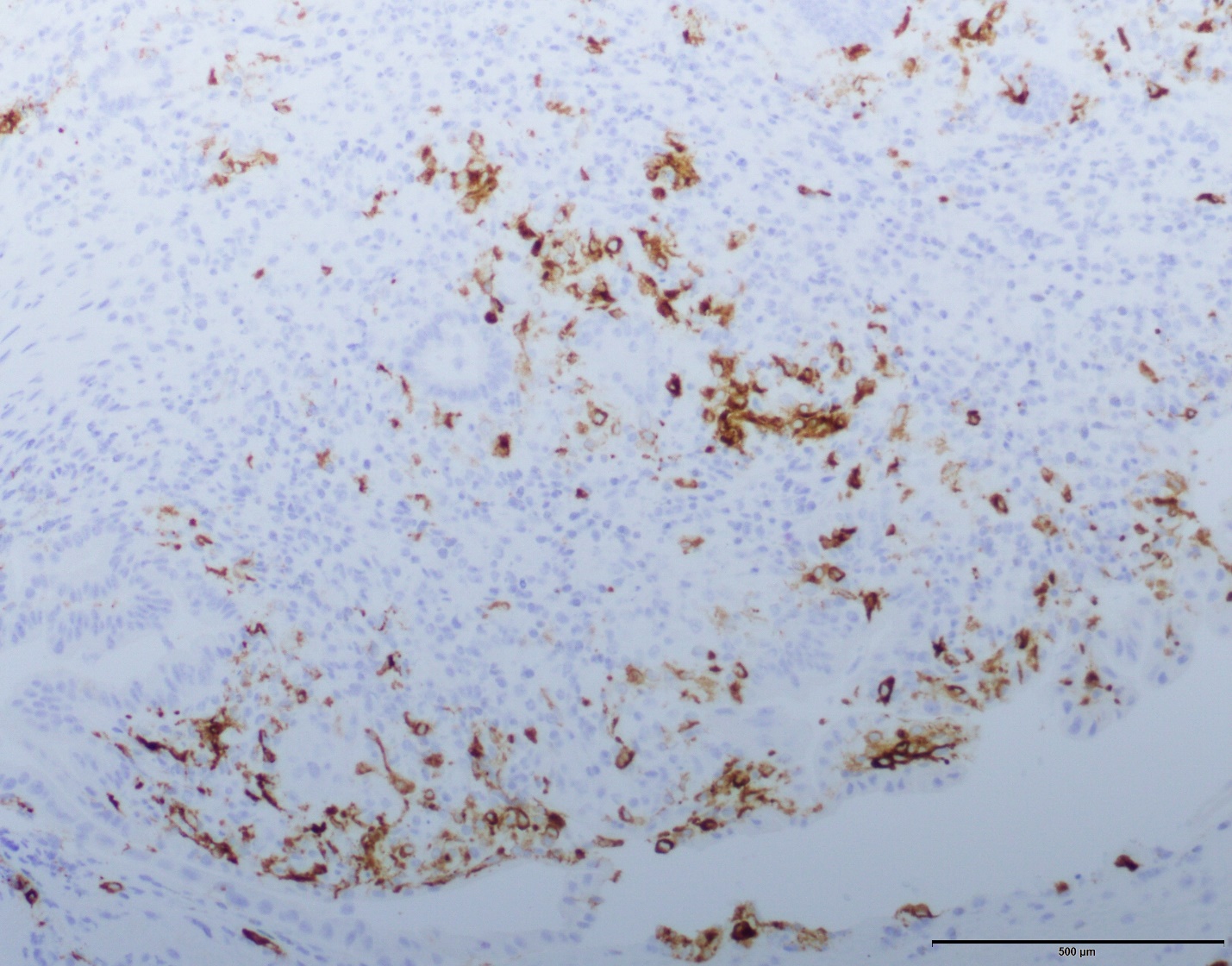
The patient is a preterm newborn who has an extensive erythematous to violaceous macular papular eruption. The biopsy is diagnostic of Langerhans cell histiocytosis characterized by predominantly dermal-based superficial and deep coalescing nodules of well-differentiated Langerhans cells. There is minimal epidermotropism. The predominant cell population exhibits an indeterminate histiocytic cell phenotype. In particular, the histiocytic cells exhibit classic cytologic features of a Langerhans cells and like a Langerhans cells are positive for CD1a, CD4 and S100. However there is significant immunoreactivity for CD68 and the majority of the cells do not express langerin. In this regard, it is reasonable to use the designation of indeterminate cell histiocytosis recognizing that there is a minor cell populace showing the typical phenotypic profile encountered in Langerhans cell histiocytosis associated with Birbeck granules i.e. the cells are langerin, CD1a, CD4 and S100 positive. Other markers that are positive include positivity for CD31 and the monocyte-derived dendritic cell marker CD11c characteristic for any monocyte derived dendritic cell neoplasm. The dominant localization of the histiocytic elements within the dermis is a cardinal hallmark of indeterminate cell histiocytosis as opposed to the very striking epidermotropic pattern that one sees in the more common langerin positive counterpart.
Indeterminate cell histiocytosis is recognized as a form of Langerhans cell histiocytosis and hence it is not surprising that in this case a minor subset of the neoplastic histiocytes show a classic Langerhans cell phenotype characterized by langerin positivity. Some authors would consider the indeterminate cell as a more mature Langerhans cell that is destined to leave the skin and migrate to the lymph node. BRAF-V600E mutations are rarely seen in indeterminate cell histiocytosis while it is seen in 50% of cases of more phenotypically conventional Langerhans cell histiocytosis. Conversely the ETV3-NCOA2 translocation is seen in indeterminate cell histiocytosis. The definitive diagnosis of ICH requires a combination of clinical presentation, histology and immunohistochemistry. Langerin (CD207), a monoclonal antibody against Birbeck granules, is the main differentiating marker that distinguishes indeterminate cell histiocytosis from Langerhans cell histiocytosis while S100 and CD1a positivity are the two key markers that separate the histiocytopathies into Langerhans cell histiocytosis versus non-Langerhans cell histiocytosis.