Case 1: Catastrophic Parvovirus B19 Endothelialitis in an Immunocompetent Host
Case 3: Juvenile Temporal Arteritis: A Case Report.
Case 4: Pancreatic Panniculitis as an Initial Presentation of Acinar Cell Carcinoma of the Pancreas
Case 5: Primary Cutaneous Blastic Plasmacytoid Dendritic Cell Neoplasm
Case 6: Acute Hemorrhagic Edema of Infancy
Case 7: Cocaine Associated Retiform Purpura
Case 10: Multiple Cutaneous Ulcers Associated With Bevacizumab Therapy
Case 11 A Case of Generalized Eruptive Histiocytosis in a 23-Year-Old Man
Case 12 Multicentric Castleman's Disease, Mixed Type
Case 13 Subcutaneous Panniculitis-like T cell Lymphoma
Case 14 Juvenile Dermatomyositis presenting as an Elbow and Knee rash
Case 15 Post Transplantation IRF Trans location + ALCL
Case 18: COVID-19 Vaccine Associated Cutaneous Lymphomatoid Reactions
Post Transplantation IRF Trans location + ALCL
Case author: Cynthia M Magro, MD
Contributing authors: Martha Torres, MD, Esther Chang, MD, Luke Olsen, MD, & Shivakumar Subramaniyam, MD
An 81-year-old male received a heart transplant in 1998 for idiopathic cardiomyopathy. The procedure was uneventful without any immediate complications. He was treated with azathioprine (50 mg) and cyclosporine (25 mg) for long-term immunosuppression with a brief period of concurrent prednisone in the distant past. Other than mild cyclosporine-related renal insufficiency, his clinical course was unremarkable. In November 2014, he presented with a history of an expanding neck lesion. Physical examination revealed a 2.2 cm non-painful nodule on the right neck. The patient was otherwise asymptomatic. An excisional biopsy of the nodule was performed. A PET scan was performed in January 2015 to rule out an occult malignancy but was negative for metastatic disease. Azathioprine was removed from his medication regimen as he was considered to be at low-risk for rejection. Clinical follow-up showed no evidence of disease progression as of the time of manuscript submission in March 2015.
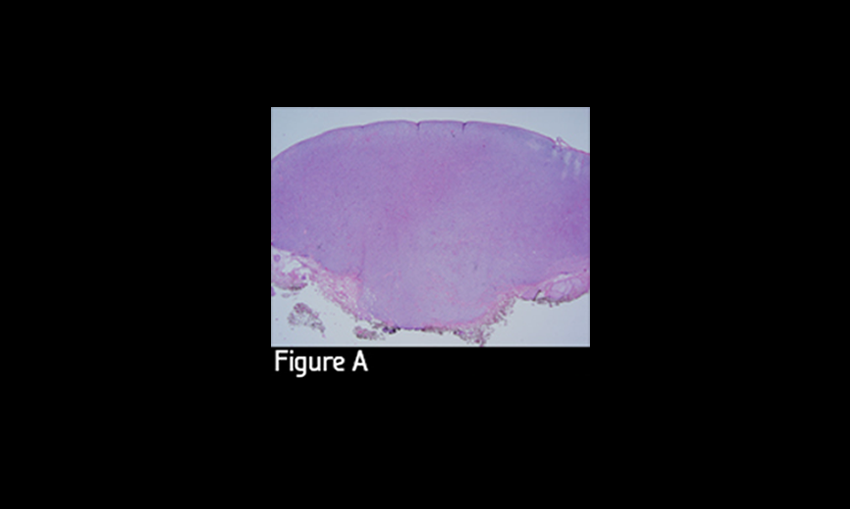
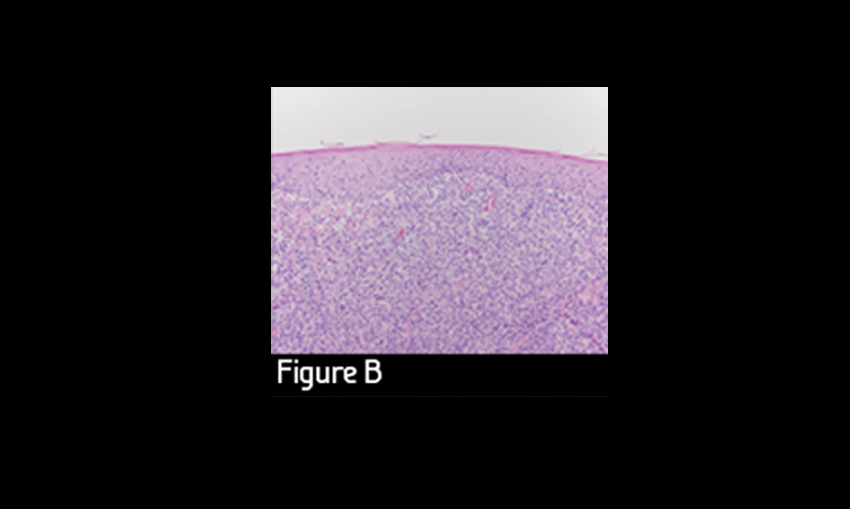
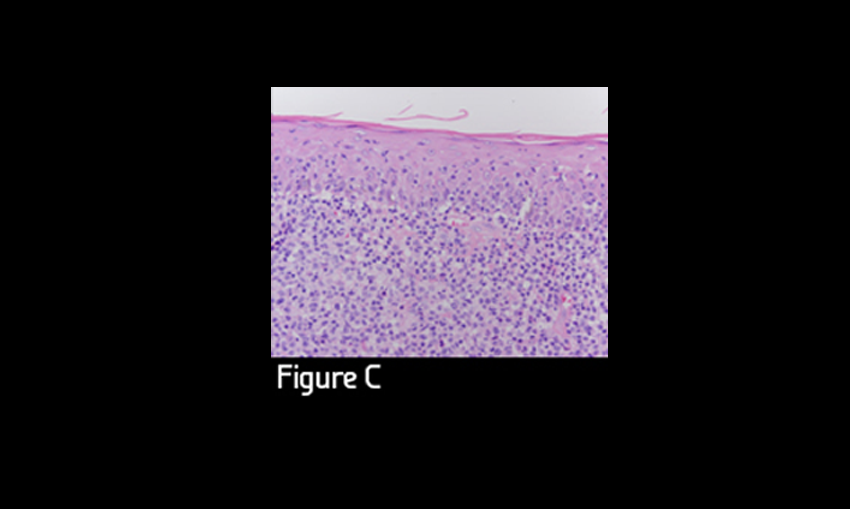
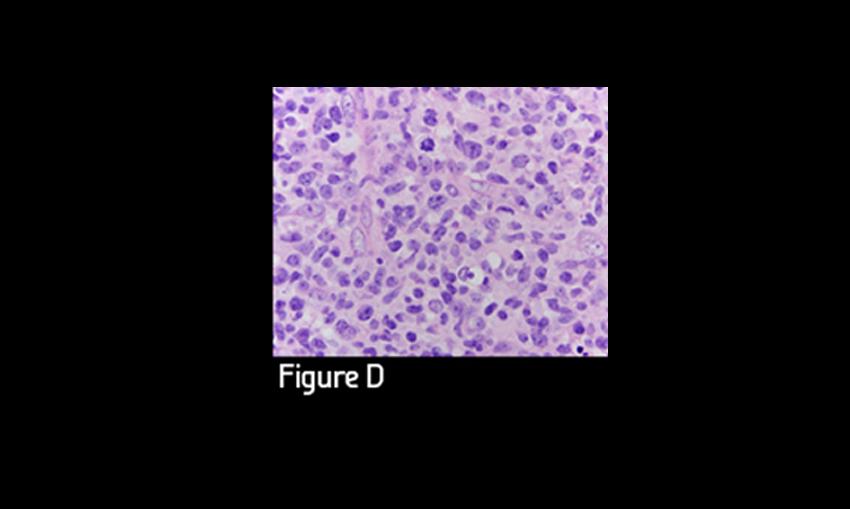
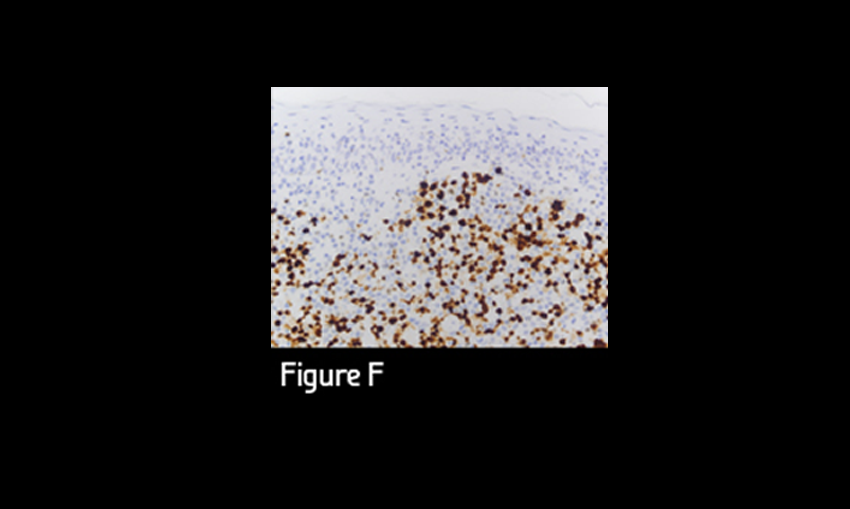
The excision of the right neck nodule revealed an effacing nodular atypical mononuclear cell infiltrate spanning the papillary and reticular dermis. There was no grenz zone separating the infiltrate from the overlying epidermis (Figure A, B). The epidermis was diffusely infiltrated in a passive epidermotropic fashion by small to intermediate sized atypical lymphocytes exhibiting a cerebriform morphology (Figure C). In contrast, the populace in the dermis was comprised of large (20-30 um) relatively monomorphic transformed-appearing cells with round to oval nuclei and conspicuous nucleolation; cytoplasms were moderately abundant (Figure D). Mitoses were abundant within the dermal population. There was a relative paucity of other inflammatory cell elements.